
Medical plastics like PLA, PETG, ABS, HIPS, and polyamide show different levels of compatibility with medical sterilization methods. Researchers test these materials using various approaches, such as ethanol, chlorine, hydrogen peroxide plasma, autoclave, and dry heat, to ensure safety and performance.
- Recent updates in AAMI TIR17:2024:
- Offer guidance on material interactions with sterilization.
- Stress the need to understand these interactions for proper selection.
- Influence choices during device development.
Key Takeaways
- Understanding polymer compatibility with sterilization methods is crucial for patient safety and device reliability.
- Selecting the right plastic for each sterilization method can prevent device failure and harmful chemical release.
- Regulatory compliance is essential; manufacturers must follow guidelines like FDA regulations and ISO standards.
- Using compatibility charts helps engineers quickly assess which plastics work best with different sterilization methods.
- Ongoing education and consultation with material experts support best practices in medical device development.
Why Medical Device Material Compatibility Matters?
Safety and Performance Implications
Medical device material compatibility plays a crucial role in ensuring patient safety and device reliability. When manufacturers select materials for medical devices, they must consider how those materials interact with sterilization methods. Incompatible materials can degrade, leading to early device failure and potential harm to patients. Some plastics withstand repeated sterilization cycles, which extends device life and reduces the risk of adverse outcomes. Others may break down, releasing harmful substances or losing structural integrity.
Note: Material degradation can result in device malfunction, which may cause serious health risks for patients.
Common issues linked to incompatible polymers include:
- Medical plastics that degrade during sterilization may release toxic compounds.
- Plasticizers like phthalates, especially DEHP, can leach out and cause toxicity or endocrine disruption.
- Vulnerable populations, such as neonates, face higher risks from exposure to these substances.
- Metabolites from plasticizers can be more harmful than the original compounds, affecting organs and cell health.
The FDA emphasizes the importance of evaluating materials for biocompatibility and biological responses. The table below summarizes key points from FDA guidance:
| Evidence Description | Source |
|---|---|
| The FDA highlights the necessity of evaluating materials for biocompatibility and biological responses when in contact with the human body. | FDA Safety of Metals |
| Manufacturers assess biocompatibility by evaluating potential adverse biological responses from device materials. | FDA Safety of Metals |
| The FDA’s evaluation process includes reviewing materials used in devices to ensure safety and effectiveness. | FDA Basics of Biocompatibility |
Regulatory Compliance and Standards
Regulatory agencies require manufacturers to demonstrate medical device material compatibility with sterilization methods. These requirements help ensure that devices remain safe and effective throughout their intended use. Manufacturers must follow strict guidelines and standards, including:
- FDA regulations under the Code of Federal Regulations (CFR) Title 21, which include Quality System Regulation (21 CFR Part 820) for sterilization processes.
- European Union Medical Device Regulation (MDR) and standards such as ISO 13485 and ISO 14937.
- International standards like ISO 11135 for ethylene oxide sterilization, ISO 11137 for radiation sterilization, and ISO 17665 for moist heat sterilization.
- Validation of sterilization processes to confirm effectiveness and consistency.
- Biocompatibility testing, often assessed through ISO 10993.
Manufacturers who meet these standards reduce the risk of device recalls and regulatory penalties. Adhering to these guidelines also supports global market access and patient trust.
Overview of Medical Sterilization Methods
Healthcare facilities rely on several medical sterilization methods to ensure the safety and effectiveness of medical devices. These methods include steam sterilization, dry heat, radiation, ethylene oxide, and hydrogen peroxide gas sterilization. Each method interacts differently with medical plastics, influencing device performance and longevity.
- Autoclaving (Steam Sterilization): Uses heat and pressure to eliminate microorganisms.
- Vaporized Hydrogen Peroxide Gas Sterilization: Provides a low-temperature option for heat-sensitive devices.
- Radiation: Includes gamma, electron beam, and X-ray sterilization.
- Ethylene Oxide Gas Sterilization: Offers compatibility with many polymers but raises concerns about emissions.
The table below summarizes how common sterilization methods affect medical plastics:
| Sterilization Method | Effects on Plastics |
|---|---|
| Steam Sterilization | High temperatures (121–132 °C) can destroy polymer structures, adversely affecting properties. |
| Ethylene Oxide Sterilization | Compatible with most polymers; does not lead to structural or color changes. |
| Ionizing Radiation | Affects physical and chemical properties; changes depend on polymer composition and irradiation conditions. |
| Gamma Irradiation | Can cause chain scission or crosslinking, affecting clarity, color, or mechanical strength. |
| Electron Beam Sterilization | Limited penetration; some plastics may become brittle or discolored under high doses. |
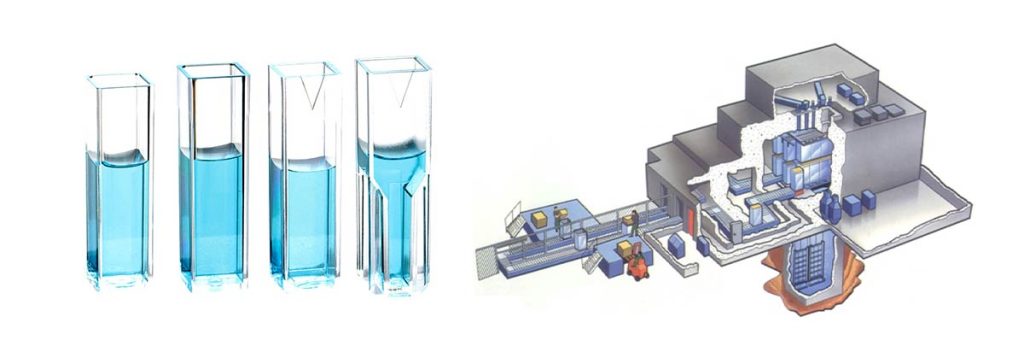
Ethylene Oxide (EtO) Sterilization
Ethylene oxide gas sterilization remains a popular choice for heat-sensitive medical plastics. This method works as a direct alkylating agent, inactivating microorganisms by reacting with their cellular components. The high reactivity and diffusivity of ethylene oxide ensure thorough sterilization. Studies show that while ethylene oxide can cause minor chemical modifications in polymers, these changes do not increase cytotoxicity. For example, poly(ether ether ketone) (PEEK) maintains its chemical integrity after ethylene oxide sterilization, though some thermal changes may occur due to the removal of residual gas. Most polymers experience minimal structural or color changes, making this method suitable for a wide range of devices.
Gamma Radiation Sterilization
Gamma radiation sterilization uses high-energy photons to penetrate and sterilize medical devices. This method can significantly alter the mechanical and chemical properties of plastics. Polymers such as PMMA and UHMWPE may undergo irreversible structural changes from free radical generation, which can limit their clinical use. Polyvinyl chloride (PVC) often experiences crosslinking and chain scission, while polycarbonate (PC) may lose clarity. Polypropylene (PP) can show changes in morphology and melting temperature, especially when sterilized in air. Polyurethane (PU) may generate harmful compounds under gamma exposure, raising safety concerns.
E-Beam Sterilization
E-Beam sterilization, performed using electron beam irradiation equipment, delivers high-energy electrons to sterilize devices quickly. This method can cause molecular weight reduction in polymers like PTFE, leading to loss of strength and integrity, especially in the presence of oxygen. Some materials, such as polypropylene homopolymer and chlorobutyl rubber, may lose tensile strength due to chain scission. However, certain polymers like polyolefin elastomer and ABS can benefit from cross-linking, which improves their mechanical properties. E-Beam sterilization can also enhance wear resistance and fatigue strength in select materials, depending on the dose and environmental conditions.
Tip: Selecting the right sterilization method depends on the specific polymer and the desired device performance. Always consider how each method may impact the material’s structure and function.
Medical Plastics Compatibility with Sterilization Methods
EtO-Compatible Polymers
Ethylene oxide sterilization remains a preferred method for many medical plastics due to its gentle process and broad material compatibility. This chemical sterilization technique works well with a wide range of plastics, preserving both safety and performance. Medical device manufacturers often select EtO-compatible plastics to ensure device longevity and maintain structural integrity after repeated sterilization cycles.
The following table highlights common medical plastics and their compatibility with ethylene oxide sterilization:
| Material | Ethylene Oxide (EtO) Compatibility |
|---|---|
| Cyclo Olefin Copolymer (COC) | Good |
| Cyclo Olefin Polymer (COP) | Good |
| Ethylene Chlorotrifluoroethylene (ECTFE) | Good |
| Ethylene Propylene Diene Monomer (EPDM) | Good |
| Ethylene Tetrafluoroethylene (Tefzel – ETFE) | Good |
| Fluorinated Ethylene Propylene (FEP) | Good |
| High Density Polyethylene (HDPE) | Good |
| High Heat Polycarbonate (PC) | Good |
| Linear Low Density Polyethylene (LLDP) | Good |
| Low Density Polyethylene (LDPE) | Good |
| Olefinic Thermoplastic Elastomer (TPO) | Good |
| Perfluoro Alkoxy (PFA) | Good |
| Perfluoroelastomer (FFKM) | Good |
| Polyamide (Nylon) | Good |
| Polyamide Thermoplastic Elastomer (TPA) | Good |
| Polycarbonate (PC) | Good |
| Polychlorotrifluoroethylene (PCTFE) | Good |
| Polydimethyl Siloxane (PDMS) | Good |
| Polyetheretherketone (PEEK) | Good |
| Polyethylene (PE) | Good |
| Polymethyl Methacrylate (PMMA) | Good |
| Polyoxymethylene (Delrin) | Good |
| Polyphenylene Sulfide (PPS) | Good |
| Polyphenylsulfone (PPSU) | Good |
| Polypropylene (PP) | Good |
| Polystyrene (PS) | Good |
Note: These plastics retain their mechanical properties and color after EtO sterilization, supporting device longevity and safety.
Despite its broad compatibility, ethylene oxide sterilization presents several challenges:
- Health risks from EtO gas exposure require strict controls.
- Environmental concerns arise due to emissions.
- The process is time-consuming, especially during the aeration phase.
- Specialized equipment and significant financial investment are necessary for compliance.
- Toxicity of EtO demands careful handling to protect workers and patients.
Medical device manufacturers must weigh these factors when choosing EtO-compatible plastics for their products.
Gamma-Compatible Polymers

Gamma radiation sterilization offers deep penetration and effective microbial inactivation, making it suitable for many medical plastics. This method supports the longevity and safety of devices by ensuring thorough sterilization. However, not all plastics respond equally to gamma irradiation. Some materials maintain their performance, while others degrade after repeated cycles.
The table below lists plastics with high compatibility for gamma sterilization:
| Material | Compatibility with Gamma Irradiation |
|---|---|
| Aluminum | Good |
| Cyclo Olefin Copolymer (COC) | Good |
| Cyclo Olefin Polymer (COP) | Good |
| Ethylene Chlorotrifluoroethylene (ECTFE) | Good |
| Ethylene Propylene Diene Monomer (EPDM) | Good |
| Ethylene Tetrafluoroethylene (Tefzel – ETFE) | Good |
| High Density Polyethylene (HDPE) | Good |
| High Density Polypropylene (HDPP) | Good |
| Polycarbonate (PC) | Good |
| Polystyrene (PS) | Good |
Tip: Gamma-compatible plastics like COC, COP, and HDPE are often selected for single-use devices and packaging due to their stability under irradiation.
However, gamma sterilization can cause several issues in medical plastics:
- Radiation-induced degradation leads to discoloration and loss of end-use properties.
- Crystalline plastics show significant degradation at high radiation doses.
- Amorphous plastics tolerate higher doses but may undergo crosslinking.
- Hydrophobic polyurethanes lose 12-30% of molecular weight and 12% of tensile strength after irradiation.
- Hydrophilic polyurethanes experience even greater losses, with up to 50% decrease in tensile strength.
- Surface roughness increases, affecting device performance and longevity.
- Chain scission and crosslinking alter the mechanical properties of plastics.
- The extent of degradation depends on the chemical structure and radiation dose.
Medical device engineers must consider these factors to ensure the longevity and safety of gamma-sterilized plastics.
E-Beam-Compatible Polymers
E-Beam sterilization uses high-energy electrons to sterilize medical plastics quickly and efficiently. This method works well for many plastics, especially when rapid turnaround is needed. E-Beam sterilization supports device longevity and maintains safety when the right materials are chosen.
The following table shows plastics with good compatibility for E-Beam sterilization:
| Polymer | Compatibility |
|---|---|
| Cyclo Olefin Copolymer (COC) | Good |
| Cyclo Olefin Polymer (COP) | Good |
| Ethylene Chlorotrifluoroethylene (ECTFE) | Good |
| Ethylene Propylene Diene Monomer (EPDM) | Good |
| Ethylene Tetrafluoroethylene (Tefzel – ETFE) | Good |
| High Density Polyethylene (HDPE) | Good |
| High Heat Polycarbonate (PC) | Good |
| Linear Low Density Polyethylene (LLDP) | Good |
| Low Density Polyethylene (LDPE) | Good |
| Olefinic Thermoplastic Elastomer (TPO) | Good |
| Perfluoro Alkoxy (PFA) | Good |
| Perfluoroelastomer (FFKM) | Good |
| Polyamide Thermoplastic Elastomer (TPA) | Good |
| Polycarbonate (PC) | Good |
| Polystyrene (PS) | Good |
| Polysulfone (PSU) | Good |
| Polyphenylene Sulfide (PPS) | Good |
| Polyphenylsulfone (PPSU) | Good |
| Polydimethyl Siloxane (PDMS) | Good |
| Polyethylene (PE) | Good |
| Polymethyl Methacrylate (PMMA) | Good |
Note: E-Beam sterilization is ideal for plastics that require fast processing and minimal heat exposure.
Selecting E-Beam-compatible plastics involves several challenges:
- Chain scission and crosslink cleavage can reduce mechanical integrity.
- Some plastics, such as PTFE, show significant damage after irradiation.
- ABS and PVDF have fair compatibility but may not withstand higher doses.
- ETFE performs well but needs post-sterilization evaluation.
- The presence of labile linkages in certain plastics increases vulnerability.
- E-Beam may not penetrate dense materials as effectively as gamma irradiation.
- Changes in properties, such as decreased osteoinductivity and altered porosity, can affect device performance.
Medical device designers must evaluate these factors to ensure the longevity, safety, and sterilization compatibility of their products. High performance polymers and rigid medical grade plastics often provide the best results for demanding applications.
Callout: Always test plastics for sterilization compatibility before finalizing material selection. This step ensures device safety, performance, and regulatory compliance throughout the product lifecycle.
Comparing E-Beam, Gamma, and EtO Sterilization
Mechanisms and Impact on Medical Device Materials
Sterilization methods use different mechanisms to eliminate microorganisms from medical devices. Ethylene oxide (EtO) acts as a chemical agent, penetrating device surfaces and reacting with cellular components. Gamma radiation uses high-energy gamma rays to disrupt DNA, while E-Beam employs high-energy electrons for rapid sterilization. Each method impacts materials in unique ways. EtO can pose sustainability challenges and carries risks due to its classification as a human carcinogen. Gamma radiation may cause material degradation over time, affecting clarity and strength. E-Beam disrupts DNA efficiently but can also alter polymer structures.
| Sterilization Method | Mechanism | Impact on Materials |
|---|---|---|
| Ethylene Oxide (EtO) | Chemical | Classified as a human carcinogen, sustainability challenges, potential for explosive failures. |
| Gamma Radiation | High-energy gamma rays | Effective but can cause material degradation over time. |
| E-Beam | High-energy electrons | Disrupts DNA of microorganisms, effective but may also lead to material changes. |
Advantages and Limitations
Each sterilization method offers distinct advantages and limitations for medical devices. E-Beam provides a rapid, dry process at ambient conditions and leaves no residuals, but requires specialized equipment and has limited penetration depth. Gamma sterilization suits high-volume production and leaves no residues, but handling radioactive materials and potential polymer degradation present challenges. EtO excels with complex geometries and sensitive materials, yet its toxicity and flammability require long aeration and strict controls.
| Sterilization Method | Advantages | Limitations |
|---|---|---|
| E-Beam | Rapid process, effective at eliminating microorganisms, no residuals left, dry process at ambient conditions | Requires specialized equipment, potential degradation of certain plastics, limited penetration depth |
| Gamma | Highly effective, suitable for high-volume production, no residuals | Requires careful handling of radioactive materials, potential polymer degradation, rigorous regulatory compliance |
| EtO | Effective for complex geometries, good penetration | Toxic and flammable, long aeration required, progressively prohibited in some regions |
Both E-Beam and Gamma methods are recognized by the FDA as established sterilization modalities, supporting regulatory acceptance for medical devices.
Typical Applications in Medical Devices
Manufacturers select sterilization methods based on device type, material, and regulatory needs. E-Beam sterilization is common for drug containers, sponges, bandages, labware, catheters, syringes, pipette tips, bottles, and test tubes. Gamma sterilization works well for medical devices that require deep penetration, especially when packaging or product density is not a concern. EtO is preferred for devices with embedded electronics and heat-sensitive components.
| Sterilization Method | Applications |
|---|---|
| E-Beam | Drug containers, Sponges, Bandages, Labware, Catheters, Syringes, Pipette tips, Bottles, Test tubes and swabs for coronavirus testing |
| EtO | Devices with embedded electronics |
| Gamma Ray | Medical devices requiring deep penetration without concern for packaging or product density |
E-Beam sterilization has scaled rapidly in recent years, increasing throughput for low-density products and improving cost-effectiveness for medical devices.
Practical Guidance and Compatibility Reference Table
Quick Reference Chart for Medical Plastics
A well-designed compatibility chart helps engineers and manufacturers quickly assess which plastics work best with different sterilization and disinfection methods. The most effective charts use a table format to display over 50 polymers, showing how each responds to various processes. Important factors include the type of sterilization, plastic type, chemical class, temperature, exposure time, and mechanical stress. These factors influence how plastics withstand sterilization and disinfection cycles.
| Polymer Name | Steam | EtO | Gamma | E-Beam | VHP | Disinfection Agents |
|---|---|---|---|---|---|---|
| Polypropylene (PP) | Good | Good | Fair | Fair | Good | Good |
| Polycarbonate (PC) | Fair | Good | Good | Good | Good | Good |
| PETG | Poor | Good | Good | Good | Fair | Good |
| HDPE | Poor | Good | Good | Good | Fair | Good |
| ABS | Poor | Good | Fair | Fair | Fair | Good |
| Nylon (PA) | Fair | Good | Fair | Fair | Good | Good |
| PMMA | Poor | Good | Fair | Fair | Fair | Good |
| PSU | Good | Good | Good | Good | Good | Good |
| PPSU | Good | Good | Good | Good | Good | Good |
| COC | Poor | Good | Good | Good | Good | Good |
| COP | Poor | Good | Good | Good | Good | Good |
Reliable data for these charts comes from sources like the Medical Chemical Compatibility Chart and reputable chemical compatibility guides. These resources evaluate corrosion resistance and help select the right materials for testing.
Selection Tips for Device Manufacturers
Manufacturers can improve patient safety and device performance by following best practices when choosing plastics for medical device development. The following tips support effective sterilization and disinfection methods:
- Match the plastic to the sterilization method. For example, use polypropylene or polycarbonate for autoclaving, PETG or HDPE for gamma, and ethylene oxide as a universal fallback. Vaporized hydrogen peroxide is a growing FDA-recognized option.
- Confirm the grade of plastic. FDA food contact approval does not guarantee suitability for healthcare. Always verify the medical grade.
- Use Kydex and Boltaron only for disinfection, not for sterilization cycles.
- Validate packaging processes with Installation Qualification, Operational Qualification, and Performance Qualification. This ensures packaging integrity after sterilization and disinfection.
- Test materials for integrity and strength. Use distribution testing to confirm compliance.
- Select materials that withstand sterilization and maintain traceability to verified suppliers.
- Follow Unique Device Identification standards for labeling and traceability.
- Align packaging and material choices with quality management systems for ongoing compliance.
Tip: Consider the type of medical application, temperature, and exposure time when selecting plastics. Proper selection reduces the risk of embrittlement and failure during sterilization and disinfection.
Conclusion
Selecting the right medical plastic for each sterilization method ensures device safety, regulatory compliance, and reliable performance. Recent research highlights several key factors:
- Material compatibility influences safety and compliance.
- Complex designs can limit sterilant penetration.
- Global standards support device effectiveness.
- Sterilization choices affect costs.
- Environmental impact matters for sustainability.
Engineers should use compatibility charts and reference updated standards like AAMI TIR17:2024. Ongoing education and consultation with material experts help maintain best practices in medical device development.
FAQ
What Factors Determine Polymer Compatibility with Sterilization Methods?
Material composition, crystallinity, and additives influence how a polymer reacts to sterilization. Temperature resistance and chemical stability also play key roles. Engineers must review data sheets and test materials before final selection.
Can a Single Polymer Suit All Sterilization Methods?
No single polymer works perfectly with every sterilization method. Some plastics withstand heat, while others resist chemicals or radiation. Manufacturers often choose materials based on the device’s intended sterilization process.
Why Do Some Plastics Change Color After Sterilization?
Gamma and E-Beam sterilization can break chemical bonds in plastics. This process sometimes causes discoloration or yellowing. The effect depends on the polymer’s structure and the radiation dose.
How Can Manufacturers Ensure Regulatory Compliance?
Manufacturers follow standards like ISO 11135, ISO 11137, and AAMI TIR17:2024. They validate sterilization processes and test for biocompatibility. Documentation and traceability help meet FDA and international requirements.
Are There Sustainable Alternatives to Traditional Sterilization Methods?
Yes. Vaporized hydrogen peroxide and low-temperature plasma offer eco-friendly options. These methods reduce emissions and energy use. Manufacturers increasingly consider sustainability when selecting sterilization processes.
