
Pharmaceutical manufacturers face constant challenges from bioburden in active pharmaceutical ingredients (APIs) and excipients. Electron beam irradiation now offers a modern solution for sterilization, targeting contamination risks with precision. Recent years show remarkable adoption rates:
- In 2023, over 15 billion single-use medical devices required sterilization, with 28% using electron beam sterilization.
- Hospitals in North America increased use of irradiation-based sterilization to 42%.
- More than 2.5 million tons of packaged food received electron beam irradiation, marking a 33% growth.
Process development, validation, and regulatory compliance remain essential for safe and effective use.
Key Takeaways
- Electron beam irradiation offers a fast and effective way to sterilize pharmaceutical products, ensuring safety without harmful chemical residues.
- Regular bioburden testing is crucial for maintaining the quality and efficacy of active pharmaceutical ingredients (APIs) and excipients.
- Careful material assessment and dose optimization are essential steps to ensure that electron beam irradiation does not degrade sensitive compounds.
- Compliance with regulatory standards, such as ISO 11137, is necessary to ensure the safety and effectiveness of the sterilization process.
- Consulting with experts during equipment selection and process validation helps maintain high safety and quality standards in pharmaceutical manufacturing.
Bioburden Control in Pharmaceuticals
Bioburden Definition
Bioburden refers to the total viable aerobic count of microbial contamination present in a sample. Scientists assess bioburden through specific assays before final sterile filtration. Bioburden testing plays a crucial role in quality control, especially for sterile products. It helps manufacturers evaluate microbial contamination and determine if further sterilization is necessary. Microbial contamination can arise from several sources during pharmaceutical manufacturing. Common contributors include:
- Raw materials such as active pharmaceutical ingredients, excipients, and solvents, which may become contaminated during harvesting, processing, or storage.
- The production process, including mixing, filling, and packaging, which presents multiple opportunities for contamination.
- Human handling and environmental factors that introduce microorganisms into the product.
- Equipment cleanliness and facility design, which can significantly affect bioburden levels.
Regulatory guidelines define acceptable bioburden levels for APIs and excipients. The following table summarizes key standards:
| Source | Guideline | Key Points |
|---|---|---|
| USP Chapter <1115> | Bioburden Control of Nonsterile Drug Substances | Focus on microbial control throughout production; emphasis on water activity and cleaning measures. |
| European GMP Guide Annex 1 | Bioburden Monitoring | Requires monitoring prior to sterilization; establishes working limits for contamination. |
| Title 21 CFR | Bioburden Testing for Medical Devices | Regulates bioburden testing for medical devices in the US. |
| ISO 11737 | Global Bioburden Testing | Provides international standards for bioburden testing. |
Impact on APIs and Excipients
Different types of bioburden, including microbial contaminants and their toxins, can affect the stability and efficacy of APIs and excipients. Microorganisms such as gram-positive bacteria, molds, yeasts, and spore-forming bacteria often originate from natural materials. The table below shows common sources:
| Microbial Type | Source of Contamination |
|---|---|
| Gram-positive bacteria | Natural materials (e.g., gum acacia) |
| Molds | Natural materials (e.g., starches) |
| Yeasts | Natural materials |
| Spore-forming bacteria | Natural materials |
Microbial toxins, including exotoxins and endotoxins, can persist through manufacturing. Heat-stable exotoxins may remain in the final product, posing safety risks. Certain molds produce mycotoxins that compromise product quality. High levels of microorganisms due to bioburden can lead to spoilage or reduced efficacy of pharmaceutical products over time. Regular bioburden testing ensures that APIs and excipients remain safe and effective throughout their shelf life.
Electron Beam Irradiation Technology
Mechanism and Safety
Electron beam irradiation uses high-energy electrons to achieve sterilization in pharmaceutical materials. The process involves accelerating electrons and directing them onto the target, where they penetrate the surface and disrupt the DNA of microorganisms. This disruption leads to cell death or prevents replication, ensuring effective sterilization. The following table summarizes the mechanism and efficiency of electron beam irradiation:
| Evidence Type | Description |
|---|---|
| Inactivation Mechanism | Ionizing radiation, including electron beam irradiation, disrupts microbial DNA, leading to cell death or inability to replicate. |
| Dosimetry | Studies evaluated bacterial suspensions as biological indicators for low-energy electron irradiation, determining inactivation doses for specific bacteria. |
| Sterilization Efficiency | A minimum dose of 25 kGy is required for effective sterilization of microorganisms using accelerated electrons. |
Electron beam sterilization delivers precise irradiation in seconds. The process leaves no harmful chemical residues, making it safer for pharmaceutical applications. It minimizes material degradation and preserves the quality of APIs, excipients, and medical devices. The technology meets ISO certification standards and offers a greener alternative to traditional radiation sterilization methods such as gamma and ethylene oxide sterilization.
Tip: Electron beam irradiation works best for low and medium density products. It is not suitable for larger or denser packages due to limited penetration depth.
Safety remains a top priority in radiation sterilization. Risk assessments help manufacturers understand how changes in irradiation sources affect product quality and safety. These assessments identify differences between electron beam irradiation and other radiation sources, guiding further empirical testing. The process requires careful monitoring to ensure that irradiation does not compromise the integrity of pharmaceutical materials.
Low energy electron irradiation (LEEI) can effectively inactivate pathogens in liquid solutions with a layer thickness below 150 μm. The antigens of irradiated viruses and bacteria remain largely intact, which can elicit protective immune responses in animal models. However, scaling beyond research applications presents challenges due to limitations in experimental setups.
Suitability for APIs and Excipients
Electron beam irradiation demonstrates compatibility with many APIs and excipients. Reviews on the effects of gamma and electron beam irradiation provide insights into the radiation stability of pharmaceuticals. Each new compound requires assessment for radiation stability, emphasizing the need for extensive testing. Analytical techniques detect radiation-induced degradation, ensuring comprehensive stability assessments.
| Evidence Type | Description |
|---|---|
| Radiation Effects | Reviews on the effects of gamma and electron-beam irradiation provide insights into the radiation stability of pharmaceuticals. |
| Stability Assessment | Each new compound must be assessed for radiation stability, indicating the need for extensive testing based on available data. |
| Analytical Tools | Various analytical techniques are necessary to detect radiation-induced degradation, ensuring comprehensive stability assessments. |
Electron beam sterilization suits low and medium density products. The following table compares penetration capabilities of different radiation sterilization methods:
| Sterilization Method | Penetration Capability | Suitable Materials | Limitations |
|---|---|---|---|
| Electron Beam | Poor compared to gamma | Low and medium density | Not feasible for larger or denser packages |
| Gamma Radiation | High | Various materials | N/A |
| X-rays | High | Full pallets, uniform treatment | N/A |
Manufacturers must evaluate the compatibility of electron beam irradiation with each API and excipient. The process preserves the quality of most pharmaceutical materials, but some compounds may degrade under irradiation. Extensive testing and analytical evaluation ensure that radiation sterilization does not compromise product safety or efficacy.
- Electron beam irradiation offers rapid and residue-free sterilization.
- Electron beam sterilization minimizes material degradation.
- Radiation sterilization provides a greener alternative to traditional methods.
- Electron-beam irradiation requires careful dose optimization for each material.
- Radiation sterilization standards guide risk assessments and quality control.
Process Development Steps
Developing an effective electron beam irradiation for bioburden control in APIs and excipients requires a systematic approach. Each step in the process ensures that pharmaceutical products meet safety and quality standards. The following sections outline the critical steps involved in process development, from initial material assessment to ongoing validation and monitoring.
Material Assessment
Material assessment forms the foundation of the electron beam irradiation. Scientists evaluate the compatibility of APIs and excipients with radiation exposure. They consider how each material responds to irradiation and identify any risks of degradation. The assessment also includes reviewing dose requirements and understanding the effects of irradiation on product stability.
| Criteria | Description |
|---|---|
| Material Compatibility | Assessment based on the response of materials to radiation exposure. |
| Dose Requirements | Determining the right dose to minimize material degradation. |
| Effects of Irradiation | Understanding how different materials perform under radiation exposure. |
Material assessment presents several challenges. Teams must address material compatibility, design complexity, regulatory compliance, cost, and environmental impact. They often compare the product’s history with gamma sterilization to predict its suitability for electron beam irradiation. Initial evaluation metrics such as product dimensions, mass, and required doses help determine if the material fits the process.
Note: Early testing during product development can prevent complications later in the sterilization process. Decisions made with sterilization in mind support smoother process validation and regulatory approval.
Dose Optimization
Dose optimization is essential for achieving effective sterilization while preserving product quality. Each API and excipient has unique properties that influence its response to irradiation. Scientists conduct specific testing to establish the minimum effective dose and the maximum allowable dose for safety. They use strategies such as transforming liquids into solids, adding free radical scavengers, and purging oxygen with inert gases to improve irradiation outcomes.
- Gamma irradiation and electron beam irradiation both kill microorganisms by breaking chemical bonds and producing free radicals.
- Quality control methodologies ensure that the sterilization process does not compromise product efficacy.
- Regulatory guidelines and literature provide decision trees for implementing irradiation in pharmaceutical manufacturing.
Teams must establish a tight dose range for irradiation. They balance the need for microbial inactivation with the risk of material degradation. Routine testing verifies that the selected dose achieves the desired level of sterilization without affecting product stability.
Equipment Selection
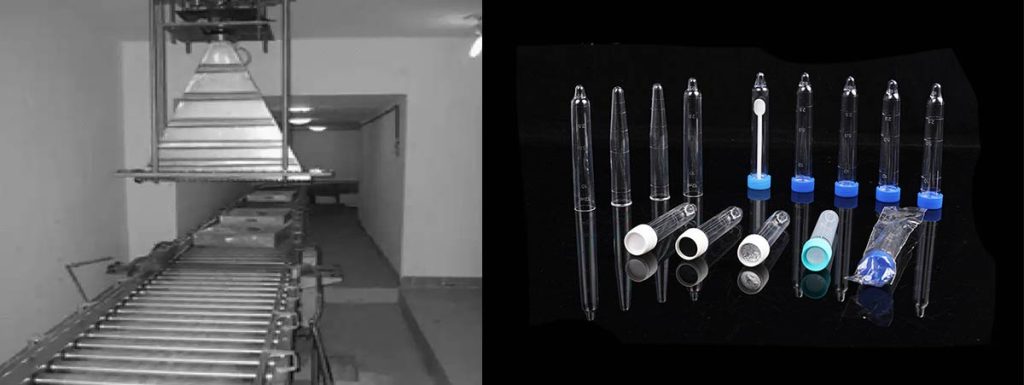
Selecting the right electron beam irradiation equipment is a critical step in the process. The equipment must match the material type, desired modifications, and required dose. Experts assess project needs and recommend suitable equipment for APIs, excipients, single-use pharmaceutical containers, and biological implants.
| Key Factor | Description |
|---|---|
| Defining Project Requirements | Clearly outline material type, desired modifications, and required dose for accurate processing. |
| Consulting with Facility Experts | Experts assess project needs, recommend doses, and ensure compliance with safety protocols. |
| Budgeting and Cost Considerations | Evaluate costs for materials and services, balancing budget constraints with long-term benefits. |
Electron beam irradiation equipment varies in design and capability. Some systems handle single-use containers and vials, while others process biological implants or certain APIs. Facility experts play a vital role in equipment selection, ensuring that the chosen system meets safety and regulatory standards. Budgeting and cost considerations also influence equipment choices, as teams must balance immediate expenses with long-term benefits.
Tip: Consulting with facility experts during equipment selection helps ensure compliance with safety protocols and regulatory requirements.
Validation and Monitoring

Validation and monitoring confirm that the electron beam irradiation consistently produces sterile products. The process includes installation qualification (IQ), operational qualification (OQ), and performance qualification (PQ). Each stage verifies that equipment operates correctly and meets predefined criteria.
| Step | Description |
|---|---|
| 1 | Develop a validated product according to ANSI/AAMI/ISO 11137 requirements. |
| 2 | Establish the maximum acceptable dose as per ANSI/AAMI/ISO 11137-1:2006. |
| 3 | Provide production-representative samples and manage the validation process. |
| 4 | Conduct pre-sterilization bioburden controls and routine assessments. |
Validation protocols follow international standards such as ISO 13485 and AAMI TIR17:2008. The customer collaborates with the irradiator, providing samples and managing the project. The irradiator ensures compliance with ISO standards and performs necessary testing. Routine monitoring includes bioburden controls and ongoing assessments to maintain process integrity.
Alert: Consistent validation and monitoring protect product safety and support regulatory compliance throughout the sterilization process.
Electron Beam Sterilization: Benefits and Limitations
Comparison to Other Methods
Pharmaceutical manufacturers use several sterilization techniques to control bioburden. Electron beam sterilization stands out for its speed and efficiency. The following table compares electron beam sterilization, gamma radiation sterilization, and steam sterilization:
| Method | Efficacy | Cost-Effectiveness |
|---|---|---|
| Electron beam sterilization | Fast process, high SAL, minimal damage to materials | Cost-effective, immediate access to sterilized products |
| Gamma radiation sterilization | Superior penetration, effective for larger items | Higher operational costs, but validated processes |
| Steam sterilization | Effective for heat-resistant materials | Generally low cost, but limited for heat-sensitive products |
Electron beam sterilization processes items in seconds. Gamma radiation sterilization works well for large or dense products. Steam sterilization remains suitable for materials that tolerate heat. Each method offers unique benefits for medical device sterilization and pharmaceutical applications.
Advantages
Electron beam sterilization provides several advantages for radiation sterilization in APIs and excipients. The process enhances operational efficiency and reduces time to market. It causes minimal oxidative damage and preserves the original quality of materials. The following table highlights key advantages:
| Advantage | Description |
|---|---|
| Efficiency and Speed | EBI processes items quickly, enhancing operational efficiency and reducing time to market. |
| Minimal Damage | It causes minor oxidative damage and minimal color change, maintaining the original quality of materials. |
| Precision and Safety | EBI is highly precise, leaves no chemical residues, and does not induce radioactivity, ensuring safety for both the environment and consumers. |
| Material Compatibility | EBI is effective on a wide range of materials, including dense ones, making it versatile for various industrial uses. |
Scientific studies show that electron beam sterilization has the shortest process cycle among recognized sterilization methods. Products receive scanning for seconds and can be released as sterile within 30 minutes. Both electron beam and X-ray methods serve as viable alternatives to gamma radiation sterilization for polymers and other materials. Radiation sterilization by electron beam does not leave chemical residues, supporting safety for consumers and the environment.
Tip: Electron beam sterilization offers immediate access to sterile products, which helps streamline pharmaceutical manufacturing.
Drawbacks
Despite its benefits, electron beam sterilization presents some limitations for radiation sterilization in pharmaceutical applications. Not all materials are compatible with sterilization by radiation. Restrictions exist for batteries and certain polymers. The table below outlines documented drawbacks:
| Drawback | Description |
|---|---|
| Material Compatibility | Not all materials are radiation-compatible. Restrictions for batteries and some polymers. |
Electron beam sterilization has limited penetration compared to gamma radiation sterilization. This limitation affects the suitability of radiation sterilization for larger or denser packages. Manufacturers must conduct thorough testing to ensure that APIs and excipients remain stable after exposure to radiation. Radiation sterilization by electron beam requires careful dose optimization and ongoing monitoring to maintain product safety and efficacy.
Alert: Always perform testing before implementing electron beam sterilization for new materials to avoid unexpected degradation.
Radiation Sterilization: Regulatory Considerations
Compliance Requirements
Regulatory agencies set strict rules for radiation sterilization in pharmaceutical manufacturing. These agencies include the FDA and EPA in the United States. The FDA inspects facilities that use sterilization to ensure they follow recognized standards. The EPA enforces regulations for facilities that emit certain chemicals during sterilization, such as ethylene oxide.
A variety of international and regional standards guide the use of radiation sterilization. The table below lists key agencies and standards:
| Region | Regulatory Agency/Standard |
|---|---|
| North America | AMI ST 32 “Guideline for Gamma Radiation Sterilization” |
| AAMI ST 31 “Guideline for Electron Beam Radiation Sterilization of Medical Devices” | |
| International | ISO 11137 “Sterilization of health care products – requirements for validation and routine control – radiation sterilization” |
| ISO 9001; ISO 9002; ISO 9004 | |
| Europe | BS EN 552 “Sterilization of medical devices – validation and routine control of sterilization by irradiation” |
Manufacturers must comply with several requirements for electron beam sterilization. These include:
- Following FDA standards for medical devices (21 CFR Part 820) and drugs (21 CFR Parts 210 and 211).
- Meeting ISO 13485 for quality management systems.
- Adhering to ISO 11137 for radiation sterilization of health care products.
- Defining a clear sterility assurance level for each product.
- Ensuring all personnel receive proper training in sterilization and radiation safety.
- Performing regular audits and ongoing dose determination.
- Conducting sterility testing and validation of radiation sterilization processes.
Note: Regular sterility testing and dose audits help maintain compliance and product safety.
Documentation
Proper documentation proves that a facility meets all regulatory requirements for radiation sterilization. Each step in the sterilization process must be recorded and reviewed. The table below outlines essential documents:
| Documentation Type | Description |
|---|---|
| Validation Reports | Show compliance, including dose mapping and microbiological validation. |
| Compliance Records | Track periodic revalidations and sterility dose audits. |
| ISO Standards | Demonstrate adherence to ISO 11137 and ISO 13485. |
Facilities must keep detailed records of sterility testing, validation, and ongoing monitoring. These records support audits and inspections by regulatory agencies. Accurate documentation ensures that the sterility assurance level is maintained for every batch. Regular updates to documentation reflect changes in processes or regulations. Sterility testing results, validation reports, and compliance records all play a role in demonstrating ongoing control of the radiation sterilization process.
Tip: Well-organized documentation makes audits smoother and helps maintain high standards for radiation sterilization.
Case Studies
API Applications
Researchers have explored electron beam irradiation for sterilizing active pharmaceutical ingredients (APIs). They observed that doxorubicin-loaded nanoparticles maintained excellent stability after exposure to doses ranging from 10 to 35 kGy. No changes appeared in physicochemical parameters, and a dose of 15 kGy proved sufficient for sterilization without causing radiolysis of doxorubicin.
The following table summarizes findings for common APIs:
| API | Irradiation Dose (kGy) | Observations on Physicochemical Properties |
|---|---|---|
| Diclofenac | 25 | No significant changes in FT-IR spectra; melting point decreased by 0.5 °C. |
| 50 | Color changed from white to cream-like; physicochemical properties remained stable. | |
| 400 | Melting point decreased to 286.0 °C; high radiation stability observed. | |
| Aceclofenac | 25 | No change in melting point; physicochemical properties remained stable. |
| 50 | Color changed from white to cream-like; physicochemical properties remained stable. | |
| 400 | Melting point decreased to 151.0 °C; high radiation stability observed. |
Scientists also tested drug-loaded PBCA nanoparticles. These particles showed excellent stability at doses between 10 and 35 kGy. No radiolysis of doxorubicin occurred at 15 kGy, confirming the method’s safety for sensitive compounds.
Excipients Applications
Electron beam irradiation has demonstrated effectiveness in sterilizing pharmaceutical excipients. Researchers found that a dose of 10 kGy could eliminate bacteria with a culture cycle of five days in a medium. The process showed minimal impact on the color of mineral pigments, which are sometimes used in pharmaceutical formulations.
A study indicated that 10 kGy electron beam irradiation could effectively kill bacteria with a culture cycle of 5 days in a medium. The research demonstrated that electron beam irradiation has potential applications in sterilization, particularly for microbial contamination, while having minimal impact on the color of mineral pigments used in frescoes.
Manufacturers can use electron beam irradiation to control microbial contamination in excipients without altering their appearance or performance. This approach supports the production of safe and high-quality pharmaceutical products.
Conclusion

Pharmaceutical teams can implement electron beam irradiation for bioburden control by following these steps:
- Assess material compatibility and stability.
- Optimize the irradiation dose for each product.
- Select appropriate equipment and consult experts.
- Validate and monitor the process according to standards.
Validation, safety, and regulatory compliance remain essential. Electron beam sterilization offers a reliable and efficient option for pharmaceutical manufacturing.
FAQ
What Is the Main Advantage of Electron Beam Irradiation for Pharmaceuticals?
Electron beam irradiation sterilizes products quickly and leaves no chemical residues. This method helps maintain the quality of APIs and excipients. It also supports faster production cycles compared to traditional sterilization methods.
Can Electron Beam Irradiation Damage Sensitive Pharmaceutical Materials?
Some sensitive materials may degrade under electron beam irradiation. Scientists recommend testing each API or excipient before full-scale use. Analytical tools help detect any changes in stability or appearance.
How Does Electron Beam Sterilization Compare to Gamma Radiation?
| Feature | Electron Beam | Gamma Radiation |
|---|---|---|
| Speed | Very fast | Slower |
| Penetration | Lower | Higher |
| Residues | None | None |
Electron beam works best for low and medium density products. Gamma radiation suits larger or denser items.
Is Electron Beam Sterilization Safe for Workers and the Environment?
Facilities use strict safety protocols to protect workers. Electron beam systems do not make products radioactive. The process produces no harmful emissions, making it environmentally friendly.
What Regulatory Standards Govern Electron Beam Sterilization?
Regulatory agencies require compliance with standards such as ISO 11137 and FDA guidelines. Facilities must document validation, routine monitoring, and staff training. These steps ensure product safety and regulatory approval.
