

Operating electron beam irradiation equipment demands strict attention to safety. This technology offers rapid processing, high material compatibility, and no hazardous emissions. Facilities can deliver sterilization doses within seconds and process multiple truckloads each day. Unlike gamma sterilization, electron beam systems use clean grid power and avoid radioactive materials, enhancing both safety and sustainability. Step-by-step procedures and robust safety protocols ensure reliable results and protect personnel.
Key Takeaways
- Always wear appropriate personal protective equipment (PPE) to minimize risks when operating electron beam irradiation equipment.
- Perform thorough area checks and ensure all safety interlocks are functional before starting the equipment to maintain a safe working environment.
- Regularly calibrate the equipment and monitor emission parameters to ensure consistent sterilization results and prevent errors.
- Carefully load materials and conduct dose audits to achieve uniform exposure during the sterilization process, enhancing product quality.
- Follow structured shutdown procedures and conduct routine maintenance to ensure the equipment operates safely and effectively over time.
Startup Safety
Personal Protection
Operators must prioritize personal protection before activating electron beam irradiation equipment. They should always wear appropriate personal protective equipment (PPE) to minimize risk.
- Operators use dosimeters to monitor their exposure levels during all emission phases.
- PPE includes a personal radiation dosimeter, especially when there is concern about exposure to penetrating ionizing radiation.
- Protective clothing, gloves, and eye protection further reduce risk from accidental emission.
Tip: Regularly check dosimeter readings to ensure exposure remains within safe limits.
Area Preparation
Proper area preparation ensures a controlled environment for safe operation. Operators inspect the workspace for any unauthorized personnel or obstacles. They verify that all shielding barriers are in place and that warning signs are visible.
Before startup, operators perform pre-startup checks to confirm reduced pressure in the vacuum chamber. This step prevents contamination and supports stable emission. Gradual filament heating is essential to avoid thermal shock:
- Heat the filament at a rate of 5–10°C per minute.
- Hold the target temperature steady for 10–20 minutes to allow even heating and release of adsorbed gases.
These steps help maintain optimal emission conditions and protect sensitive components.
Safety Interlocks
Regulatory agencies require multiple safety interlocks for electron beam irradiation equipment. These interlocks prevent accidental emission and ensure operator safety. The table below summarizes key requirements:
| Requirement | Description |
|---|---|
| Door Interlocks | Each door must have at least two safety interlocks. One disconnects energy supply when opened. |
| Access Panel Interlocks | Each access panel must have at least one safety interlock. |
| Resumption Control | After an interlock triggers, a specific control resumes operation. |
| Component Failure | Failure of one component cannot disable more than one safety interlock. |
Operators must verify all interlocks before initiating emission. This step ensures the system will halt emission if any access point is breached, maintaining a high level of safety.
Electron Beam Irradiation Equipment Setup
Power and Emission
Operators begin by initializing the linear accelerator and the power supply. The process starts with a thorough inspection of the electron beam irradiation equipment. They check that all power connections are secure and that the main control panel displays normal status indicators. The operator then activates the main power switch, which energizes the system and prepares it for emission.
The emission process requires careful control. Operators gradually increase the filament current to reach the desired emission level. This step prevents sudden surges that could damage sensitive components. The system monitors the vacuum chamber to ensure optimal conditions for emission. Operators observe the emission current and voltage, making adjustments as needed to stabilize the beam. The emission must remain steady to guarantee consistent results during processing.
Note: Operators should never leave the equipment unattended during emission. Continuous supervision helps detect irregularities early and prevents unsafe conditions.
The emission phase also involves activating the beam shutter. This device controls when the electron beam reaches the product area. Operators synchronize the shutter with the conveyor or product handling system. They verify that the emission only occurs when products are in position, reducing unnecessary exposure and conserving energy. The emission stops automatically if any safety interlock is triggered, ensuring immediate protection for personnel.
System Calibration
Accurate calibration ensures that the electron beam irradiation equipment delivers the correct dose during emission. Operators follow a series of steps to calibrate controls and monitoring devices:
- The system interrupts the emission based on the charge measured by a monitor detector.
- The monitor unit (MU) module integrates the collected signal and calculates the corresponding MU value.
- The calculated MU is compared to the preset MU after each emission pulse.
- The emission is interrupted if the calculated MU exceeds the preset value.
- Signal collection is corrected for temperature and pressure after each emission pulse.
- A recombination correction strategy is applied to account for dose-rate dependent recombination effects.
Operators use specialized components for calibration. The current transformer (ICT) uses a Super MuMetal® toroid and a secondary winding made from 50 Ω coaxial cable. A custom differential amplifier and a commercial flash analog-to-digital converter provide accurate readout. Calibration uses a sub-microsecond current pulser, which is traceable to electrical standards through an in-house electrometer.
Tip: Regular calibration checks help maintain the reliability of emission measurements and prevent dose errors.
Material Loading
Proper material loading is essential for uniform exposure during emission. Operators prepare products by assessing their internal configuration and bulk density. They use dose maps to measure how emission distributes within the product. Validation runs confirm the accuracy of these dose maps before routine processing begins.
Operators perform sterilization dose audits before production and at regular intervals. These audits ensure that the emission remains consistent and effective. Product placement relative to the beam is carefully studied. Operators adjust the orientation and spacing of items to optimize electron penetration and achieve even emission across all surfaces.
- Accurate dose distribution supports consistent sterilization results.
- Performance qualification is conducted on multiple containers to account for variations in dose distribution.
- Operators document each step to maintain traceability and support quality assurance.
Reminder: Uniform loading and regular audits help prevent under- or over-exposure during emission, protecting both product quality and safety.
The setup phase for electron beam irradiation equipment lays the foundation for safe and effective emission. Careful attention to power, calibration, and material handling ensures that each emission cycle meets strict safety and quality standards.
E-Beam Sterilization Process
Dose Selection
Selecting the correct dose stands as the foundation of the e-beam sterilization process. Operators determine the required dose based on the type of product, its density, and the level of microbial contamination. For the sterilization of medical devices, the dose must meet strict regulatory standards to ensure safety and effectiveness. Operators use dose mapping to identify the minimum and maximum doses received by different parts of the product. This mapping helps prevent underdosing, which could leave harmful microorganisms, and overdosing, which might damage sensitive materials.
The e-beam sterilization process uses high-energy electrons to break down the DNA of bacteria, viruses, and other pathogens. Operators adjust the dose by changing the beam current, conveyor speed, or exposure time. They monitor these parameters closely to maintain consistent results. Regular validation runs confirm that the selected dose achieves the desired level of sterility without compromising product quality.
Tip: Operators should always verify dose distribution with dosimeters placed at critical points within the product load.
Electron Beam Transmittance
Electron beam transmittance describes how deeply the electrons penetrate the product during the e beam sterilization process. This property depends on the energy of the electron beam and the density and thickness of the product. Higher energy beams can reach deeper layers, making them suitable for bulkier items. Operators must balance beam energy to achieve effective sterilization throughout the product while avoiding unnecessary exposure.
The e-beam sterilization process relies on precise control of electron beam transmittance. Operators use depth-dose profiles to analyze how the dose changes as electrons move through the product. These profiles help identify areas that may receive less exposure and require adjustment. For example, products with complex shapes or varying densities may need special orientation or multiple passes to ensure uniform sterilization.
A clear understanding of electron beam transmittance allows operators to optimize the e-beam sterilization process for a wide range of applications, from food packaging to pharmaceuticals.
Product Scanning
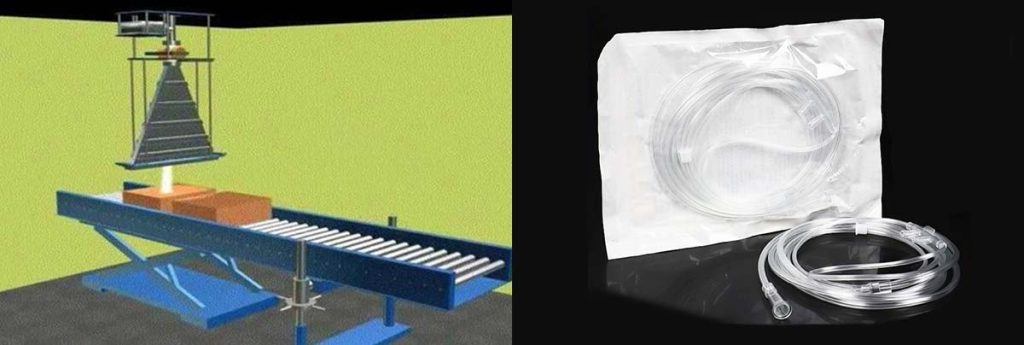
Product scanning ensures that every surface and internal area receives the correct dose during the e beam sterilization process. The electron beam irradiation equipment creates a curtain of electrons that sweeps across the conveyor belt or product tray. Operators configure the system to match the size and shape of the products, adjusting the scanning width and speed as needed.
The following table summarizes key components and concepts involved in the scanning process:
| Component | Description |
|---|---|
| Common Terminology | Terms used in e beam sterilization, such as “dose mapping” and “depth-dose profile” |
| E-beam Overview | Introduction to electron beam technology and its principles |
| Process Configuration | Setup and arrangement of the e beam system for optimal coverage |
| Electron Beam Dose Distribution | How the dose spreads across the product during scanning |
| Depth-Dose Profile | Analysis of dose penetration at different product depths |
| Applications | Uses of e-beam sterilization in industries like healthcare and food safety |
| Process Validation | Steps to ensure the process meets sterilization standards |
| Technology Comparison | Comparison of e-beam sterilization with other methods, such as gamma or X-ray |
Operators monitor the scanning process in real time. They use sensors and dosimeters to confirm that the electron beam sterilization delivers the intended dose to all product areas. If the system detects any deviation, operators can adjust the scanning parameters immediately. This flexibility makes the e beam sterilization process highly reliable and adaptable.
Note: Consistent product scanning reduces the risk of incomplete sterilization and supports high throughput in industrial settings.
The e-beam sterilization process combines careful dose selection, precise control of electron beam transmittance, and thorough product scanning. These steps ensure that electron beam sterilization remains a safe, efficient, and effective method for a wide variety of products.
Monitoring and Stability
Real-Time Monitoring
Operators rely on real-time monitoring to maintain emission stability and ensure the safe operation of electron beam irradiation equipment. They track several key parameters during the e beam sterilization process. The following table highlights the most common monitoring parameters:
| Monitoring Parameter | Description |
|---|---|
| Beam Energy | Determined using electron activation, depth dose curves, and range measurements. |
| Electron Spectra | Obtained through electron scattering and spectral analysis techniques. |
| Beam Deposition | Monitored by measuring energy changes with sequential aluminum plates, without intercepting the beam. |
Technologies such as electron optical imaging, infrared thermography, and high-resolution imaging help operators detect surface defects and monitor temperature distribution. These tools provide immediate feedback, allowing quick adjustments to emission settings. Operators also use optical emission spectroscopy to analyze the elemental composition and fringe projection monitoring to inspect powder bed irregularities. Real-time data supports rapid responses to any deviation in emission or system performance.
Process Optimization
Process optimization focuses on maintaining reduced pressure and stable emission during the e-beam sterilization process. Operators use advanced high-power electron beam welding systems and simple mechanical vacuum pumps to achieve and sustain the required vacuum. The table below outlines recommended methods for maintaining reduced pressure:
| Method/Technology | Description/Benefit |
|---|---|
| Advanced High Power EB Welding | Operates at higher pressures, enabling local vacuum arrangements and reducing large chamber needs. |
| Simple Mechanical Vacuum Pump | Establishes welding vacuum with basic equipment, simplifying on-site operation. |
| Increased Tolerance to Cleanliness | Only the immediate joint area requires cleaning, streamlining preparation. |
| Reduced Pumping Time | Shortens the time needed to reach operational vacuum, increasing efficiency. |
| Elimination of Metal Vapour Risk | Maintains a positive helium flow, preventing breakdowns in the electron gun. |
Operators monitor emission parameters closely to ensure emission stability. They adjust the gun stand-off distance and maintain a positive flow of helium to protect high-value parts. These steps help prevent breakdowns and support consistent operation throughout the e-beam sterilization process.
Consistent Electron Beam Sterilization
Consistent electron beam sterilization depends on several critical factors. Operators receive proper training to optimize cycle time and capacity. Effective loading techniques ensure even distribution of instruments, which enhances exposure to the sterilizing agent. Facilities select sterilizers based on workflow and instrument usage patterns, investing in advanced technologies to improve efficiency.
- Regular monitoring of the e-beam sterilization process maintains compliance with safety standards.
- Structured training programs reduce downtime and improve operational effectiveness.
- Facilities prioritize efficiency and safety to protect patient health during the sterilization of medical devices.
Operators document each cycle, track emission stability, and review system performance. These practices ensure that the e-beam sterilization process delivers reliable results across multiple processing cycles. Stability in emission and operation supports high-quality outcomes and maintains the integrity of electron beam sterilization.
Shutdown and Maintenance
Safe Shutdown
Operators must follow a structured process to safely shut down electron beam irradiation equipment. They begin by reducing the emission current and allowing the system to cool. The operator powers down the linear accelerator and disconnects the main supply. The cathode must cool gradually to prevent thermal stress. Emergency procedures require immediate action if the system displays abnormal behavior. Operators listen, observe, report, and follow up on any unusual operation. They investigate all reports of abnormal function and include these in the facility’s quality assurance program. Medical device manufacturers must establish formal procedures for returning equipment after maintenance. They report all returned equipment to the physics group before resuming patient treatment. The physics group verifies the radiation beam if repairs may have affected beam parameters. A full review or investigation occurs when the equipment displays unusual behavior.
Tip: Operators should never skip shutdown steps, even during emergencies. Proper shutdown protects the cathode and ensures safe operation for medical device manufacturers.
Troubleshooting
Electron beam irradiation equipment may encounter several common issues during operation. Medical device manufacturers must address these problems quickly to maintain safety and efficiency. The table below summarizes frequent issues and standard troubleshooting steps:
| Issue | Troubleshooting Steps |
|---|---|
| Reduced Beam Intensity | Adjust objective lens apertures based on specimen type. Use energy filters to enhance beam intensity. Clean components like apertures and energy filters. Replace worn or damaged parts if cleaning is ineffective. |
| Overheating | Avoid running at maximum power for long periods. Gradually heat the filament during startup. Maintain reduced pressure during operations. Regularly clean filament housing and cathode assembly. Conduct service evaluations every six months. |
| Contamination | Follow strict cleaning procedures using lint-free cloths and isopropyl alcohol. Wear gloves during cleaning. Store parts in sealed containers. Use anti-contamination devices and advanced cleaning methods. |
| Irregular Focus | Adjust focus settings and inspect lenses. Experiment with spot sizes and condenser apertures. Utilize free lens control for custom spot sizes. Regularly inspect and replace damaged lenses. |
| Vacuum Conditions | Maintain routine cleaning and servicing of vacuum pumps. Implement contamination control strategies. Regularly replace and calibrate the electron source. Use magnetic shielding techniques to protect the electron beam. |
Medical device manufacturers often use field emission cathodes to improve beam stability and reduce maintenance needs. Operators must inspect the cathode regularly and replace it if performance drops. Proper troubleshooting ensures reliable operation and extends the life of the cathode.
Routine Maintenance
Routine maintenance keeps electron beam irradiation equipment safe and effective for medical device manufacturers. Operators monitor the validated sterilization process, including bioburden monitoring and sterility testing. Bioburden monitoring occurs quarterly or more often to ensure cleanliness and compare results with original validation data. Sterility testing uses a verification dose and checks product sterility, often during audits. ISO 11137 recommends initial monitoring intervals of one to three months, with quarterly checks being most common. After four successful dose audits and stable quarterly bioburden results, testing frequency may reduce to once every twelve months.
Operators clean the cathode assembly and related parts using lint-free cloths and isopropyl alcohol. They store cleaned parts in sealed containers to prevent contamination. Field emission cathodes require less frequent replacement, but operators must still check them for wear. Medical device manufacturers rely on regular maintenance to ensure safe operation and consistent sterilization results.
Note: A well-maintained cathode supports stable emission and reduces downtime for medical device manufacturers.
Conclusion

Operators maintain safety by following strict startup, operation, and shutdown procedures for electron beam irradiation equipment. They check personal protection, area preparation, and safety interlocks before each use. Training remains essential. Regulatory bodies require operators to complete written and practical exams, receive annual refresher courses, and learn radiation safety fundamentals.
| Requirement | Description |
|---|---|
| Understanding of licensee’s procedures | Operators must demonstrate understanding of the licensee’s license and operating procedures through a written or oral examination. |
| Training in equipment use | Operators must receive training in the use of radiographic exposure devices and associated equipment. |
| Practical examination | Operators must demonstrate understanding through a practical examination covering the use of radiographic exposure devices and survey instruments. |
| Annual refresher training | Licensees must provide annual refresher safety training for each operator at intervals not exceeding 12 months. |
| Fundamentals of radiation safety | Training must include fundamentals of radiation safety, including characteristics of radiation, hazards, and methods of controlling exposure. |
| Radiation detection instruments | Training must cover the use, operation, calibration, and limitations of radiation survey instruments. |
| Equipment operation | Operators must be trained in the operation and control of radiographic exposure equipment and related storage and disposal procedures. |
| Federal regulations | Training must include the requirements of pertinent Federal regulations and case histories of accidents in radiography. |
Operators use a checklist for each cycle:
- Inspect PPE and dosimeters.
- Prepare the area and verify interlocks.
- Calibrate controls and load materials.
- Monitor emission and system parameters.
- Document each step and perform routine maintenance.
Recent advancements in electron beam irradiation equipment improve precision, efficiency, and expand applications in healthcare, food, and manufacturing.
| Advancement Type | Description |
|---|---|
| Precision Improvements | Enhanced control mechanisms and variable beam energy for better adaptability in sterilization. |
| Efficiency Enhancements | Increased scalability and speed of the sterilization process without compromising product quality. |
| Expanded Applications | Adoption across various sectors including healthcare, pharmaceuticals, food, and cosmetics. |
Operators who follow protocols and receive ongoing training help facilities achieve reliable, eco-friendly sterilization. Electron beam irradiation equipment supports rapid, safe, and effective processing for many industries.
FAQ
What Factors Affect the Stability of Electron Beam Irradiation Equipment?
Stability depends on vacuum quality, temperature control, and regular maintenance. Operators monitor emission parameters and adjust settings to maintain stability. High e-beam transmittance and high performance also support long-term stability. Consistent monitoring ensures the equipment delivers reliable results during long-term operation.
How Does High E-Beam Transmittance Improve Sterilization Performance?
High e-beam transmittance allows electrons to penetrate deeper into products. This feature ensures uniform dose distribution and enhances performance. Operators achieve high performance by adjusting beam energy and product orientation. High e-beam transmittance supports stability and long-term stability in sterilization processes.
Why Is Long-Term Stability Important for Electron Beam Irradiation Equipment?
Long-term stability ensures the equipment operates safely and efficiently over time. Operators rely on long-term stability to maintain high performance and consistent sterilization. Regular calibration and maintenance help preserve stability. High e-beam transmittance also contributes to long-term stability and reliable performance.
What Maintenance Steps Support High Performance and Stability?
Operators clean and inspect the cathode, check vacuum pumps, and calibrate controls. These steps maintain high performance and stability. High e-beam transmittance and long-term stability depend on routine maintenance. Operators document each step to ensure the electron beam irradiation equipment meets performance standards.
How Can Operators Ensure Consistent Performance During Long-Term Operation?
Operators monitor emission parameters, adjust beam settings, and perform regular audits. High e-beam transmittance and stability help maintain consistent performance. Long-term stability depends on proper training and documentation. Electron beam irradiation equipment delivers high performance when operators follow strict protocols.
