

E-beam sterilization presents several challenges for drug eluting stents. Material stability and drug potency can suffer during sterilization. Low drug dosage analysis often complicates accurate measurement. PLG compound interference and mass-balance concerns, such as increased benzoic acid, may affect results. Solutions exist for each issue, ensuring safety and maintaining patient health.
Key Takeaways
- E-beam sterilization can affect the stability of materials in drug-eluting stents. Manufacturers must balance effective sterilization with maintaining material integrity to ensure patient safety.
- Drug potency may decrease during e-beam sterilization. Accurate measurement of low drug dosages is crucial to confirm that the device delivers the intended therapeutic effect.
- Shadowing effects during sterilization can lead to uneven radiation exposure. Engineers must optimize stent positioning to ensure consistent sterilization across all areas.
- Regular validation and monitoring of sterilization processes are essential. These practices help maintain compliance with regulatory standards and ensure the safety of drug-eluting stents.
- Automation in the sterilization process can enhance efficiency and reliability. Automated systems help manage production scale while maintaining high safety standards.
E-Beam Sterilization Challenges
Material Stability
E-beam sterilization affects the stability of materials used in drug eluting stents. The process exposes polymers to radiation, which can change their mechanical properties. Several mechanisms contribute to these changes:
- Chain scission breaks polymer chains, making the material weaker.
- Cross-linking forms new bonds between chains, which can increase strength or cause brittleness.
- Material decomposition leads to weight loss and the release of small molecules during biodegradation.
- Excessive irradiation may cause embrittlement and degrade polymer properties.
The degradation rates of common stent polymers depend on the irradiation dose and the environment. For example, ionizing radiation can cause chain branching and cross-linking, increasing molecular weight. It may also lead to chemical degradation and oxidation, reducing molecular weight. The table below shows how irradiation conditions affect the behavior of PLA, a common stent polymer:
| Polymer Type | Irradiation Condition | Degradation Behavior |
|---|---|---|
| PLA | Varies by dose | Strongly influenced by irradiation conditions |
Material compatibility challenges arise when the polymer structure changes. These changes can impact device performance and patient safety. Manufacturers must balance sterilization effectiveness with maintaining material integrity.
Drug Potency
E-beam sterilization can reduce the potency of drugs coated on stents. Radiation may break down active ingredients, lowering their effectiveness. Low drug dosage analysis presents a challenge because the amount of drug is often very small. Detecting these low levels requires sensitive equipment and precise methods.
When the drug degrades, new compounds may form. Some of these compounds can interfere with analysis or exceed impurity thresholds. Manufacturers must demonstrate that these impurities do not pose risks to patient safety. Accurate measurement ensures that the device delivers the intended therapeutic effect.
PLG Compound Interference
PLG-related compounds, formed during sterilization, complicate drug analysis. The presence of co-eluting radiolysis degradation products makes it difficult to detect low drug dosages. Chromatographic profiles of active substances may change, hindering accurate identification. The formation of new degradation products can increase mass-balance concerns, such as a rise in benzoic acid levels.
Tip: Regular calibration of analytical instruments helps improve detection accuracy and ensures safety for patients.
Manufacturers must address these challenges to maintain the quality and safety of drug eluting stents. Careful process control and validation help minimize risks and protect patient health.
Dose Distribution and Process Control
Stent Geometry
The geometry of drug eluting stents creates unique challenges for e-beam sterilization. Stents often have intricate designs with thin wires and small gaps. These features can cause uneven exposure to radiation. Electron beam irradiation equipment must deliver a consistent dose across the entire device. If some areas receive less radiation, sterilization may not be effective. Engineers study the stent’s shape and adjust the process to ensure every part receives the correct dose. This step helps maintain material compatibility challenges and supports patient safety.
Shadowing Effects
Shadowing occurs when parts of the stent block radiation from reaching other areas. This effect can lead to under-sterilized regions, which may compromise safety. The impact of shadowing depends on the stent’s orientation and placement during the process. Technicians use precise positioning and rotate devices to minimize shadowing. They also select irradiation containers that allow optimal exposure. These actions help protect the drug delivery function and ensure the device meets safety standards for the patient.
Advanced Dosimetry
Accurate dose measurement is essential for effective sterilization. Advanced dosimetry techniques help monitor and control the process. Experts validate these methods by considering several critical elements:
| Critical Elements in E-beam Performance Qualification |
|---|
| Internal product configuration |
| Bulk density of the product |
| Product’s placement in relationship to the beam |
| Sufficient number of irradiation containers (minimum of three) |
Technicians analyze these factors to achieve uniform dose distribution. They use sensors and dosimeters to track radiation levels. Process validation ensures that every device meets strict sterilization requirements. These steps reduce risks and support patient safety. Consistent dose control preserves drug potency and maintains the impact of the device throughout its lifetime.
Note: Regular process monitoring and validation help ensure the safety and reliability of drug eluting stents.
Device Performance and Terminal Sterilization
Mechanical Integrity
E-beam sterilization impacts the mechanical integrity of drug eluting stents. The process exposes medical devices to radiation, which can change their physical properties. Researchers observed several effects on mechanical performance:
- Increased rigidity in stent materials
- Decreased flexibility, which may affect deployment
- Enhanced barrier properties that help resist fluid penetration
- Faster decomposition when exposed to enzymes
Engineers address material compatibility challenges by testing stents before and after terminal sterilization. They rinse and flush each unit with a 70% isopropyl alcohol solution. Some protocols use ultraviolet sterilizers or add antimicrobial agents such as ProClinTM or sodium azide. Technicians mount mock arteries without deployed stents and run machines at experimental pressures and flows. This setup helps establish a baseline particle count. After sterilization, they monitor for particle spikes, especially during the initial phase of testing.
Tip: Regular mechanical testing ensures patient safety and device reliability.
Surface Changes
Radiation from e-beam sterilization causes changes on the surface of drug eluting stents. Scientists measure these changes by tracking molecular weight. The table below shows how increasing the e-beam dose affects the number average molecular weight of stent materials:
| E-beam Dose (kGy) | Number Average Molecular Weight (Da) | Relationship (1/Mn vs. Dose) |
|---|---|---|
| 0 | Initial Value | 0 |
| 50 | Decreased Value | Linear relationship observed |
Surface changes may alter drug release rates and affect the overall performance of the device. Engineers adjust design features to maintain safety and effectiveness.
Lifetime and Safety
Terminal sterilization plays a key role in the lifetime and safety of medical devices. Manufacturers use pre- and post-sterilization testing to confirm that stents meet durability standards. They record particle spikes during early testing but focus on long-term results. Design adjustments help maintain drug potency and mechanical strength. These steps protect the patient and ensure that drug eluting stents perform as intended throughout their lifespan.
Regulatory and Quality Challenges
Compliance
Regulatory bodies set strict requirements for drug-eluting stents that undergo e-beam sterilization. Agencies such as the FDA in the United States and MDR in the European Union require manufacturers to validate sterilization methods and ensure product safety. These organizations also demand risk management assessments and compliance with performance standards. The following table summarizes key regulatory requirements in major markets:
| Regulatory Body | Key Requirements |
|---|---|
| FDA (US) | Validation of sterilization methods, including dose mapping and bioburden testing. Compliance with Quality System Regulation (21 CFR Part 820). |
| MDR (EU) | Validation of sterilization processes, risk management assessments, and compliance with safety and performance standards. |
| ISO 11137 | Guidelines for the development, validation, and routine control of e-beam sterilization processes. |
Manufacturers must meet these standards to ensure that stents remain safe and effective for patients.
Documentation
Proper documentation supports compliance and demonstrates that manufacturers follow best practices. Companies must establish both minimum and maximum sterilization doses for each product. They test samples at different doses to confirm acceptable limits. Adherence to standards such as ANSI/AAMI/ISO 11137-1:2006 is essential. The table below outlines required documentation practices:
| Requirement | Description |
|---|---|
| Establishing Minimum Dose | Manufacturers must communicate the minimum sterilization dose required for their product. |
| Establishing Maximum Dose | Manufacturers must determine and communicate the maximum acceptable dose to the sterilizer. |
| Testing Samples | A range of doses must be tested on product samples to establish acceptable limits. |
| Compliance Standards | Adherence to ANSI/AAMI/ISO 11137-1:2006 is required for sterilization practices. |
Note: Accurate records help regulatory agencies verify that products meet all safety and performance criteria.
Validation Protocols
Validation protocols confirm that the sterilization process works as intended. Manufacturers use robust testing and continuous monitoring to maintain product quality. They perform dose mapping, bioburden testing, and risk assessments. Routine audits and process reviews help identify areas for improvement. Teams update protocols as new technologies and regulations emerge. These steps ensure that drug-eluting stents deliver consistent results and protect patient health.
Tip: Regular validation and monitoring support long-term reliability and regulatory compliance.
Scalability and Cost in Sterilization Process
Throughput
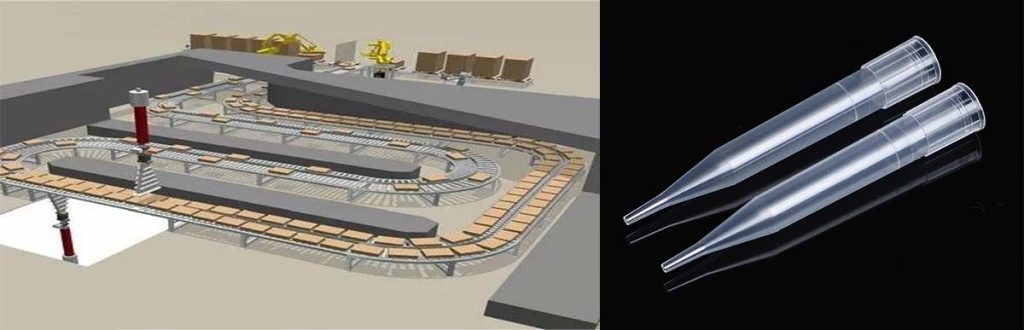
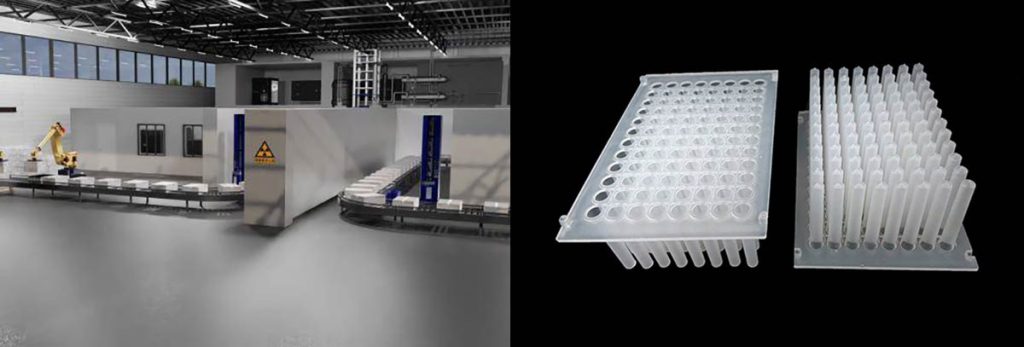
Manufacturers face several challenges when scaling up e-beam sterilization for drug-eluting devices. Many existing product designs were created for gamma sterilization, making adaptation to e-beam difficult. Industry practices often favor familiar gamma processes, which slows the adoption of new methods. Shipper box design can also limit throughput, as packaging may not allow for effective e-beam exposure. Some devices only qualify for low maximum doses, restricting flexibility in the sterilization process. These factors can slow production and increase the risk of bottlenecks.
- Existing product designs may not suit e-beam requirements.
- Industry habits favor gamma sterilization.
- Packaging often needs redesign for optimal e-beam exposure.
- Low maximum dose limits device compatibility.
Cost Efficiency
E-beam sterilization offers several cost advantages over traditional methods. Facilities do not require consumable chemicals, which reduces both procurement and disposal expenses. The process avoids the high costs linked to cobalt-60 isotopes used in gamma sterilization. E-beam facilities need less space and have simpler regulatory requirements, which lowers infrastructure costs. Products become ready for use immediately after sterilization, improving inventory management and reducing holding costs. Modular e-beam systems allow for flexible capacity adjustments, which supports cost-effective scaling.
| Cost Factor | Description |
|---|---|
| Lower Operating Costs | No chemical usage and energy efficiency reduce expenses. |
| No Isotope-Related Costs | Avoids high procurement and security costs of gamma sterilization. |
| Lower Infrastructure Costs | Smaller facility footprint and simpler compliance lower capital expenses. |
| Accelerated Turnaround | Immediate readiness of products lowers inventory holding costs. |
| Scalability | Modular systems allow flexible capacity adjustments. |
Automation
Automation helps manufacturers overcome many scalability challenges. Automated systems can optimize batch sizes and device positioning, which ensures consistent radiation exposure. Robotics can handle packaging and movement, reducing manual labor and human error. Automated monitoring systems track the sterilization process in real time, which improves safety and quality. These solutions make it easier to scale up production while maintaining high standards for drug-eluting devices.
Tip: Automation not only increases throughput but also enhances process reliability and product safety.
Conclusion
E-beam sterilization presents many challenges for drug-eluting stents. Targeted solutions help manufacturers manage material stability, drug potency, dose distribution, and regulatory compliance. Careful process control and validation protect device performance and patient safety.
Ongoing innovation in sterilization technology and quality assurance practices ensures that drug-eluting stents remain safe and effective for future patients. Manufacturers continue to improve reliability and adapt to new standards.
FAQ
What Is the Main Benefit of E-Beam Sterilization for Drug-Eluting Devices?
E-beam sterilization provides rapid processing and avoids chemical residues. This method helps maintain the integrity of drug-eluting devices. Manufacturers choose e-beam when they need fast turnaround and high sterility assurance level.
How Does Stent Geometry Affect Radiation Sterilization?
Stent geometry influences dose distribution during radiation sterilization. Complex shapes can cause shadowing, which may lead to uneven exposure. Engineers use advanced technologies and dosimetry to ensure every part of the device meets performance targets.
What Guidance Exists for Selectinga Sterilization Method?
Guidance on selecting a sterilization method comes from regulatory agencies and industry standards. Experts recommend evaluating device materials, drug stability, and intended use. Manufacturers compare methods such as e-beam, ethylene oxide sterilization, and gamma to match their development strategy.
How Do Manufacturers Ensure Sterility Assurance Level?
Manufacturers validate processes using dose mapping, bioburden testing, and routine audits. These steps provide assurance that devices meet sterility assurance level requirements. Teams monitor results and update protocols to maintain safety and effectiveness.
What Role Does Documentation Play in Meeting Performance Targets?
Documentation supports compliance and helps manufacturers achieve performance targets. Teams record every step, including testing and validation. Accurate records allow regulatory agencies to verify that drug-eluting devices meet safety standards and guidance.
