
Dose uniformity ratio (DUR) plays a critical role in ensuring sterility and maintaining product quality during ebeam sterilization. A lower DUR often means better dose consistency, which protects both safety and efficiency. Recent data show that the DUR for a new X-ray pallet configuration reaches 1.28, while gamma irradiation containers report a DUR of 1.64. Operators who monitor DUR closely can reduce risks and maintain reliable sterilization. A quick-reference checklist supports ongoing DUR management for every facility.
- DUR for X-ray pallet: 1.28
- DUR for gamma irradiation container: 1.64
Key Takeaways
- Understand the Dose Uniformity Ratio (DUR) to ensure consistent sterilization. A lower DUR indicates better dose distribution, which is crucial for product safety.
- Regularly perform dose mapping to identify areas of uneven radiation exposure. This practice helps maintain product quality and sterility.
- Calibrate and maintain electron beam equipment routinely. Proper calibration ensures accurate dose delivery and prevents unexpected variations.
- Optimize product arrangement and process parameters to improve DUR. Experimenting with stacking patterns can enhance dose uniformity and efficiency.
- Use checklists and staff training to support consistent DUR management. These tools help prevent errors and ensure reliable sterilization outcomes.
DUR in Ebeam Sterilization
DUR Definition
Dose uniformity ratio describes the relationship between the highest and lowest dose delivered to products during radiation sterilization. Operators use DUR to measure how evenly electron beam radiation treats items in a batch. A lower DUR signals that the sterilization process delivers a more consistent dose, which helps maintain sterility and product quality. Key factors influence dose uniformity ratio in ebeam sterilization:
- Product geometry affects how ionizing radiation penetrates and distributes the dose.
- Packaging density changes how much radiation each item absorbs.
- Dose mapping ensures every part of the product receives the required sterilization dose.
Understanding these factors allows facilities to optimize radiation sterilization and protect product integrity.
DUR Challenges
Maintaining a stable dose uniformity ratio presents several challenges in ebeam sterilization. Operators often encounter issues related to product density and packaging configuration. Short stack configurations improve dose distribution for dense products. Layout processing helps manage tight dose ranges for combination products. The orientation of products in containers is crucial for achieving homogeneous exposure. Dense packaging configurations complicate the conversion process, requiring higher doses and leading to wider dose distribution. These challenges can impact the effectiveness of sterilization and may require adjustments to process parameters.
Tip: Regularly review product arrangement and packaging density to minimize dose variation and improve radiation sterilization outcomes.
DUR Window
Facilities must operate within an acceptable DUR window to ensure effective sterilization. The typical range for medical device sterilization using ebeam technology is shown below:
| Parameter | Value |
|---|---|
| Dmin | 24.3 kGy |
| Dmax | 35.8 kGy |
| Dose Uniformity Ratio (DUR) | 1.4 |
Operators should monitor the dose window closely. Staying within these limits helps maintain sterility and ensures that products receive adequate electron beam radiation without exceeding safe thresholds. Consistent monitoring supports reliable radiation sterilization and protects product safety.
Recognizing DUR Problems
Signs
Operators in ebeam facilities often notice early warning signs when dose uniformity ratio begins to drift outside acceptable limits. These signs help staff identify potential issues before they affect product safety. Common indicators include inconsistent dose readings across different areas of a product batch and unexpected variations in sterilization results. Facilities that monitor areal density and packaging configuration can catch problems early. The following table summarizes key factors and their descriptions:
| Factor | Description |
|---|---|
| Areal Density | Keeping the maximum areal density of the package under 8.5 grams/cm² can help maintain tolerable DUR performance. |
| Packaging Configuration | Adjusting the configuration of products inside packaging can minimize the areal density profile presented to the beam. |
Note: Regular checks of areal density and packaging arrangement support early detection of DUR problems.
Operators also observe changes in dose mapping results. When the highest and lowest dose measurements show a widening gap, this signals a potential DUR issue. Staff should review product stacking and orientation whenever these signs appear.
Symptoms
Symptoms of dose uniformity ratio problems often become visible during routine quality checks. Products may show uneven sterilization, with some items receiving too much radiation and others too little. Staff may find that certain areas of a pallet or container fail sterility tests more frequently. These symptoms can lead to increased product rejections and delays in shipment.
Facilities sometimes report higher rates of non-conformance when DUR problems persist. Operators may notice that dose mapping results fall outside the validated range. Inconsistent color changes in dosimeters also point to uneven dose distribution. Staff should respond quickly to these symptoms to prevent compromised product safety.
Tip: Early recognition of symptoms allows operators to adjust process parameters and maintain consistent DUR performance.
Root Causes
Equipment
Operators often trace dose uniformity ratio issues to the performance and setup of electron beam irradiation equipment. This equipment uses high-speed electrons to deliver ionizing radiation for sterilization. Unlike gamma radiation, which uses photons with deep penetration, e-beam systems have limited penetration. This difference means that equipment calibration and maintenance play a major role in achieving consistent dose distribution. If the equipment fails to deliver a stable beam or if sensors drift out of calibration, the dose can vary across the product batch. Regular calibration checks help maintain the accuracy of dose delivery and support reliable radiation sterilization.
Note: Facilities should schedule routine calibration and maintenance for electron beam irradiation equipment to prevent unexpected dose variation.
Operators also monitor the alignment and energy settings of the equipment. Incorrect alignment can cause uneven exposure, while improper energy settings may result in some products receiving too much or too little dose. These factors directly impact the effectiveness of sterilization and the ability to maintain sterility.
- Key equipment-related factors affecting DUR:
- Calibration accuracy
- Beam alignment
- Energy settings
- Sensor reliability
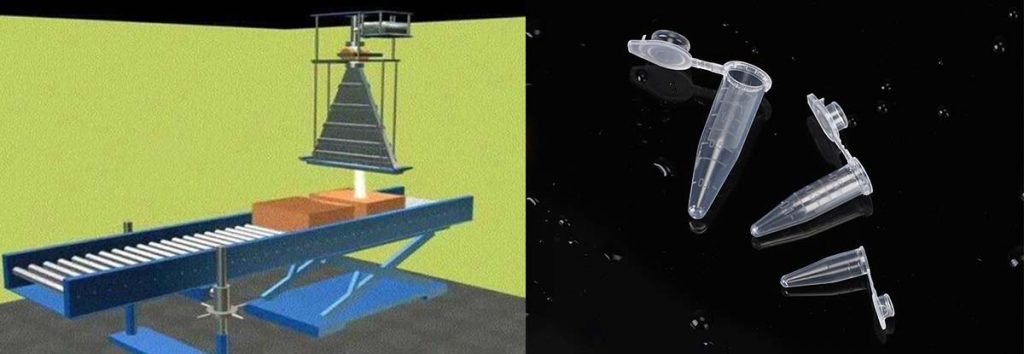
Product Arrangement

Product arrangement inside the irradiation chamber strongly influences dose uniformity ratio outcomes in ebeam sterilization. Since electrons do not penetrate as deeply as gamma rays, operators must arrange products to ensure each item receives the required dose. Placing products in individual boxes can reduce the depth of penetration needed, which improves dose distribution. Facilities often use dual e-beam systems to expose products from two sides, further enhancing uniformity.
Operators pay close attention to stacking patterns and packaging density. Dense arrangements can block the beam and create areas with lower dose, while sparse arrangements may lead to overexposure. Adjusting the orientation and spacing of products helps achieve a more uniform dose and supports effective radiation sterilization.
Tip: Testing my product in e-beam systems with different arrangements can reveal the best configuration for optimal dose uniformity.
Dose mapping plays a critical role in evaluating product arrangement. By measuring internal and surface doses, operators identify areas with dose variation and adjust the layout to improve uniformity. This process ensures that all products meet sterilization standards and maintain sterility.
Process Parameters
Process parameters such as conveyor speed, beam current, and exposure time directly affect dose delivery in radiation sterilization. Operators set these parameters based on product type and packaging characteristics. Incorrect settings can cause the dose to fall outside the required range, leading to uneven sterilization.
Facilities use dose mapping to validate process parameters. This technique measures the minimum and maximum doses received by products, helping operators adjust settings for optimal uniformity. Regular monitoring of process parameters ensures that the sterilization process remains consistent and effective.
Operators also consider the differences between gamma and ebeam sterilization when setting process parameters. Gamma radiation provides a flat penetration profile, which allows for close minimum and maximum dose requirements. E-beam systems require more precise control due to their limited penetration. Adjusting process parameters to match product and equipment characteristics helps maintain a stable dose uniformity ratio and supports reliable radiation sterilization.
Callout: Consistent process parameter management is essential for maintaining product safety and meeting regulatory standards in radiation sterilization.
Solutions
Calibration
Accurate calibration of electron beam equipment forms the foundation for consistent radiation sterilization. Facilities must perform regular calibration checks to ensure the system delivers the correct dose to every product. Calibration involves comparing measured doses to calculated values under controlled conditions. Operators use a series of tests to validate the treatment planning system for electron beams. These tests help maintain a stable dose uniformity ratio and support product sterility.
The following table outlines essential calibration tests and their tolerances:
| Test # | Objective | Tolerances |
|---|---|---|
| 8.1 | Verify absolute dose under reference conditions | 0.5% |
| 8.2 | Model verification with shaped fields | 3%/3 mm |
| 8.3 | Surface irregularities/obliquity | 5% |
| 8.4 | Inhomogeneity test | 7% |
Operators should schedule these tests routinely. Each test checks a different aspect of dose delivery, from absolute accuracy to performance with irregular surfaces. By following these best practices, facilities can prevent unexpected dose variation and maintain reliable radiation sterilization.
Tip: Regular calibration not only improves dose accuracy but also reduces the risk of product rejection due to uneven sterilization.
Dose Mapping
Dose mapping allows operators to visualize how ionizing radiation distributes across products during sterilization. This process involves placing dosimeters at various points inside the product load. After exposure, staff measure the dose at each location. Dose mapping identifies areas that receive too much or too little radiation. Operators then adjust product arrangement or process parameters to improve uniformity.
Facilities should perform dose mapping during initial validation and whenever they change product configuration. This practice ensures that every item receives the required sterilization dose. Dose mapping also helps facilities stay within the validated dose window, which protects both product quality and sterility.
A typical dose mapping workflow includes:
- Placing dosimeters throughout the product load.
- Running the sterilization cycle.
- Measuring and recording the dose at each point.
- Analyzing results to identify high and low dose regions.
- Adjusting product arrangement or process settings as needed.
Note: Consistent dose mapping supports ongoing process improvement and helps facilities meet regulatory standards for radiation sterilization.
Optimization
Optimization focuses on refining product arrangement and process parameters to achieve the best possible dose uniformity ratio. Operators experiment with different stacking patterns, packaging densities, and orientations to find the most effective setup. Adjusting conveyor speed, beam current, and exposure time can also improve dose distribution.
Expanding the acceptable dose uniformity ratio window can lead to significant efficiency gains. Facilities that optimize their processes often see reduced treatment times and improved product quality. The table below summarizes documented benefits of optimizing the DUR window in ebeam sterilization:
| Evidence Type | Description |
|---|---|
| Dose Uniformity Ratio | Expanding the DUR window improves dose delivery and reduces product damage. |
| Treatment Times | Ebeam technology shortens treatment times compared to gamma sterilization. |
| Product Quality | Optimized photon energy delivery enhances product quality and DUR. |
Operators who optimize their processes can deliver the required sterilization dose more efficiently. This approach reduces the risk of oxidation and discoloration, which protects product integrity. Facilities that maintain a stable dose uniformity ratio also improve overall radiation sterilization outcomes.
Callout: Optimization not only increases efficiency but also ensures that every product meets strict sterility requirements.
Prevention
Routine Checks
Facilities maintain dose uniformity ratio by performing routine checks throughout the sterilization process. Staff conduct dose mapping by placing dosimeters inside product loads. This step helps measure dose distribution and identifies both minimum and maximum internal doses. Operators establish an acceptable surface dose range for ongoing monitoring. Regular audits of the sterilization dose, following ANSI/AAMI/ISO 11137 standards, confirm that the dose remains consistent with the initial production run. These checks help prevent unexpected changes in dose delivery and support reliable sterilization outcomes.
Tip: Routine dose mapping and audits allow operators to catch problems early and maintain high product safety standards.
Training
Staff training plays a vital role in preventing dose uniformity ratio issues. Well-trained employees understand how to place items correctly and calibrate sterilization parameters. They also know how to monitor the process and respond to changes. The following table highlights how training impacts dose uniformity ratio:
| Training Aspect | Impact on Dose Uniformity Ratio |
|---|---|
| Proper Item Placement | Ensures uniform x-ray penetration and effective sterilization. |
| Calibration of Sterilization Parameters | Maintains required dose while achieving a consistent ratio. |
| Routine Monitoring | Confirms that sterilization conditions are met throughout the cycle. |
Facilities invest in ongoing education to keep staff updated on best practices. This approach reduces errors and improves overall sterilization quality.
Checklist
Operators use checklists to support consistent DUR management. A checklist helps staff remember key steps and maintain process control. Common checklist items include:
- Verify equipment calibration before each run
- Perform dose mapping for new product configurations
- Review product arrangement and packaging density
- Audit sterilization dose according to standards
- Document any changes in process parameters
Callout: A well-designed checklist improves efficiency and reduces the risk of missing critical steps in ebeam sterilization.
Routine checks, staff training, and checklists work together to prevent future DUR issues. Facilities that follow these best practices maintain reliable sterilization and protect product integrity.

Conclusion
Operators improve dose uniformity ratio by following clear troubleshooting steps. They calibrate equipment, map doses, and optimize product arrangement. Regular monitoring and preventive practices help maintain consistent results. Facilities use ongoing e-beam dose audits, track bioburden amounts, and perform verification dose experiments to confirm effective sterilization. A checklist and step-by-step guide support reliable DUR control.
- Ongoing e-beam dose audits
- Bioburden determination
- Verification dose experiment
Consistent attention to these steps protects product safety and ensures process efficiency.
FAQ
What Is Dose Uniformity Ratio (DUR) in Ebeam Sterilization?
Dose uniformity ratio measures the difference between the highest and lowest radiation dose received by products. Operators use DUR to check if sterilization is even and effective.
Why Does Product Arrangement Affect DUR?
Product arrangement changes how the electron beam reaches each item. Dense stacking can block radiation, while proper spacing improves dose distribution. Operators test different layouts to find the best uniformity.
How Often Should Facilities Perform Dose Mapping?
Facilities should perform dose mapping during initial validation and after any change in product configuration. Regular mapping helps operators maintain consistent dose delivery and meet safety standards.
What Are Common Signs of DUR Problems?
Operators notice inconsistent dose readings, uneven sterilization, and frequent product rejections. These signs suggest the dose uniformity ratio has moved outside acceptable limits.
How Can Staff Training Improve DUR Performance?
Staff training teaches employees how to arrange products, calibrate equipment, and monitor the process. Well-trained staff help facilities achieve better dose uniformity and reduce errors.
