

E-beam sterilization offers a precise solution for complex medical devices with embedded electronics. This technology uses a stream of electrons to quickly sterilize devices while keeping temperatures low. Sensitive electronics benefit from this approach in several ways:
- Rapid sterilization protects delicate components from prolonged exposure.
- The absence of heat and reactive gases helps preserve electronic function.
- Devices prone to thermal damage, like wearable sensors and electronic skin technologies, retain their integrity.
Key Takeaways
- E-beam sterilization quickly and effectively sterilizes complex medical devices without heat, preserving sensitive electronics.
- This method allows for rapid processing times, with some devices ready for market in as little as 2 hours, ensuring timely delivery.
- Material compatibility is crucial; not all materials withstand e-beam exposure, so careful selection is necessary for device integrity.
- E-beam technology supports the safe use of advanced applications like electronic skin, maintaining functionality and comfort after sterilization.
- Manufacturers must validate e-beam processes to ensure safety and effectiveness, following strict regulatory standards for medical devices.
E-Beam Technology in Medical Devices
What Is E-Beam?
E-beam sterilization uses high-energy electrons to eliminate microorganisms on medical devices. Electron beam irradiation equipment directs a focused beam of electrons onto the surface of the product. The electrons penetrate the material and disrupt the DNA and RNA of bacteria, viruses, and other pathogens. This process sterilizes the devices quickly and efficiently.
- E-beam sterilization uses electron accelerators, while gamma sterilization relies on radioactive isotopes.
- Both methods use ionizing radiation to destroy microorganisms, but e-beam does not involve radioactive materials, making it safer for operators and the environment.
- E-beam technology completes sterilization in seconds, while gamma sterilization takes longer.
E-beam sterilization stands out because it does not require chemicals or high temperatures. This feature makes it ideal for applications involving sensitive electronics. The process is precisely controlled, which helps maintain the integrity of advanced medical devices.
Application to Embedded Electronics
Medical devices with embedded electronics, such as wearable medical devices and electronic skin, require careful sterilization. E-beam technology offers several advantages for these applications. Electron beam irradiation equipment can sterilize devices even when they are sealed in their final shipping containers. The process inactivates microorganisms by directly damaging vital molecules or through indirect chemical reactions.
Advanced electronics in medical devices benefit from the rapid and low-temperature nature of e-beam sterilization. The technology supports a wide range of applications, including implantable sensors, diagnostic tools, and wearable devices. E-beam sterilization also proves cost-effective, especially for devices with low bulk density. The pricing structure, based on packaging size, often results in lower costs for taller boxes.
Recent advancements in e-beam technology have improved processing speed and reliability. The industry has seen a shift from gamma to e-beam sterilization, driven by economic benefits and increased capacity. Manufacturers now design products to enhance compatibility with e-beam applications, ensuring safe and effective sterilization for the latest medical electronics.
E-Beam Sterilization Process
Step-By-Step Overview
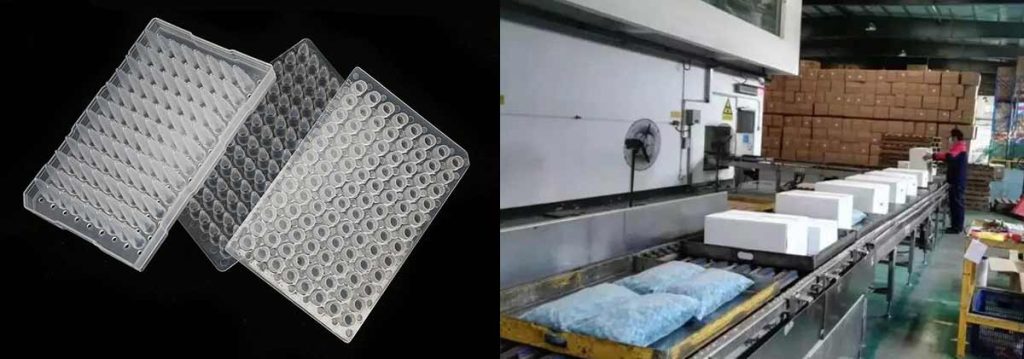
E-beam sterilization follows a precise sequence to ensure the safety and effectiveness of medical devices with embedded electronics. The process begins with the preparation of devices, which are often sealed in their final packaging. Operators load these packages onto a conveyor system that moves them into the irradiation chamber. Inside the chamber, a high-energy electron beam targets the products. The electrons penetrate the packaging and reach the devices, disrupting the DNA and RNA of microorganisms.
The irradiation step occurs rapidly, with exposure times measured in seconds. This speed limits the risk of heat buildup, which is critical for electronics and sensitive materials. After irradiation, the devices exit the chamber and undergo quality checks. The standard turnaround time for batch processing is 48 hours for market release. Some facilities can complete the process in as little as 2 hours for urgent needs.
- E-beam sterilization uses rapid irradiation to minimize thermal stress.
- The process maintains low temperatures, protecting sensitive electronics.
- Devices remain in their final packaging, reducing contamination risks.
- Turnaround times range from 2 to 48 hours, supporting fast market delivery.
Impact on Device Integrity
Medical devices with embedded electronics require careful handling during sterilization. E-beam technology preserves both the structural and functional integrity of these products. The process is suitable for complex or heat-sensitive materials, such as plastics, polymers, and coatings. Unlike gamma radiation, e-beam is gentler and limits damage to device components.
- E-beam sterilization maintains the biocompatibility of materials used in implants and prosthetics.
- The process preserves the functionality of sensitive electronics, ensuring reliable performance after sterilization.
- Devices retain their original structure, which is essential for applications in diagnostics, monitoring, and therapy.
Manufacturers rely on e-beam sterilization for wearable medical devices and advanced electronics. The technology supports the integration of e-skins and other innovative solutions, allowing for safe and effective use in clinical settings.
Electronic Skin Technologies
Electronic skin technologies, or e-skin, represent a new frontier in medical applications. These devices mimic the properties of human skin and enable advanced sensing, monitoring, and therapeutic functions. The integration of e-skins into medical devices demands a sterilization method that protects delicate adhesives and electronic components.
Researchers have studied the effects of e-beam sterilization on various acrylic skin-contact adhesives used in e-skin applications. The table below summarizes the impact on shear effect and moisture vapor transmission rate (MVTR):
| Adhesive Type | Shear Effect | MVTR Change |
|---|---|---|
| I | Significant | Significant |
| II | Minimal | Minimal |
| III | Minimal | Minimal |
| IV | Significant | Significant |
Adhesives II and III show minimal changes after e-beam exposure, making them suitable for use in electronic skin technologies. This finding supports the integration of e-skins into wearable devices and other medical applications. E-beam sterilization enables the safe processing of e-skin products, preserving their performance and comfort for patients.
Tip: Selecting the right adhesive type is crucial for maintaining the integrity of e-skin devices after e-beam sterilization.
The combination of rapid, low-temperature processing and compatibility with sensitive materials makes e-beam an ideal choice for the next generation of medical electronics.
Challenges for Embedded Electronics
Heat and Radiation Risks
Medical devices with embedded electronics face unique risks during e-beam sterilization. The electron beam delivers energy that can generate heat inside the device. Sensitive electronics may malfunction if exposed to excessive temperatures. Rapid irradiation helps limit heat buildup, but some components remain vulnerable. Microchips, sensors, and batteries often have strict thermal limits. Overheating can cause circuit failure or degrade performance.
Radiation exposure also presents challenges. The electron beam can disrupt the structure of electronic components. High doses may damage semiconductors or alter the properties of integrated circuits. Some devices require shielding or special packaging to protect critical electronics. Manufacturers must balance the need for effective sterilization with the risk of damaging sensitive parts.
Note: Careful calibration of e-beam parameters reduces the risk of heat and radiation damage to embedded electronics.
Material Compatibility
Material selection plays a crucial role in the success of e-beam sterilization for medical devices. Not all materials respond well to electron beam exposure. Some plastics and polymers may discolor, become brittle, or lose mechanical strength after irradiation. The compatibility of materials with e-beam sterilization determines the long-term reliability of medical electronics.
The table below highlights common material compatibility issues:
| Material | Compatibility Rating | Comments |
|---|---|---|
| Acrylonitrile butadiene styrene (ABS) | ★★★ | High-impact grades are less radiation resistant due to higher butadiene content. |
| Polytetrafluoroethylene (PTFE) | ★ | May be challenging to qualify at higher doses; significant damage can occur when irradiated. |
Some additional considerations include:
- E-beam sterilization may not be ideal for high-density or larger volume products due to limited penetration depth.
- Certain polymers may experience discoloration or brittleness after exposure, depending on the material and radiation dose.
Material compatibility affects both the safety and performance of medical devices. Engineers must test and qualify each material for use in e-beam applications. This process ensures that wearable medical devices and other advanced electronics maintain their function after sterilization.
Wearable Device Considerations

Wearable devices introduce further complexity to the sterilization process. These products often combine flexible electronics, adhesives, and soft polymers. Each component must withstand e-beam exposure without losing its intended properties. For example, adhesives used in wearable applications must retain their stickiness and comfort after sterilization.
Wearable medical devices require special attention to packaging and design. Thin, flexible structures may absorb energy differently than rigid devices. Uneven energy distribution can lead to incomplete sterilization or localized damage. Manufacturers often use dosimetry mapping to verify that all areas of the device receive the correct dose.
Applications such as electronic skin demand even greater precision. These devices must remain comfortable, biocompatible, and fully functional after sterilization. The integration of advanced electronics into wearable formats pushes the limits of current sterilization technology.
Tip: Early collaboration between design engineers and sterilization experts improves outcomes for wearable and flexible medical devices.
Medical applications continue to evolve, and the demand for safe, reliable sterilization methods grows. E-beam technology offers many advantages, but it also requires careful planning and validation to address the unique challenges of embedded electronics.
Solutions and Best Practices
Optimizing E-Beam Parameters
Operators must carefully select e-beam parameters to protect medical devices with embedded electronics. Dose selection plays a key role in ensuring both sterility and device safety. The maximum dose tested should be at least twice the minimum dose established for sterilization. Exceeding this ratio where possible helps confirm the device’s tolerance. The routine processing dose must not fall below the sterilization dose required for the product’s safety assurance level, nor exceed the maximum dose the product can handle. This approach supports a wide range of applications, including implantable sensors and wearable medical devices.
- The maximum dose being tested should be at least two times greater than the established minimum dose.
- The routine processing dose range cannot be lower than the sterilization dose needed for the SAL required for the product and no higher than the maximum allowable dose confirmed for the specific product.
Device Design Strategies
Engineers design medical devices with e-beam sterilization in mind. They select materials and electronics that resist radiation and heat. Packaging design also matters. Robust seals and cushioned trays protect devices during handling and shipping. Barrier materials prevent microbial contamination. Packaging should allow easy access for healthcare workers while maintaining sterility.
- Maintain sterility by ensuring seal integrity and using barrier materials.
- Protect devices mechanically with strong seals and cushioned trays.
- Support aseptic presentation through packaging that allows easy access.
These strategies help wearable applications and other advanced electronics survive the sterilization process without loss of function.
Validation and Testing
Manufacturers use strict validation and testing protocols to confirm the safety and efficacy of e-beam sterilized medical devices. They conduct seal strength, peel, and burst tests to confirm packaging integrity. Accelerated and real-time aging studies assess how packaging materials perform over time. Simulated distribution testing replicates transportation stresses. Microbial challenge and leak testing verify barrier performance.
The sterility test was conducted using the direct inoculation method, where irradiated implant samples were immersed in tryptone broth and incubated to check for microbial growth. Confirmation of growth was done by sub-culturing on tryptone soya agar plates.
These steps ensure that electronics in medical applications, including wearable devices and electronic skin, remain safe and effective for patient use.
Quality and Compliance
Safety Assurance
Quality assurance plays a vital role in e-beam sterilization for complex medical devices with embedded electronics. Manufacturers implement a range of measures to ensure that devices remain safe and effective for clinical applications. These steps help maintain the integrity of electronics and packaging throughout the sterilization process.
- Validate sealer temperature, time, and pressure to keep equipment calibrated.
- Test seal strength and integrity so packaging opens cleanly without tearing.
- Conduct distribution simulations to check packaging under different conditions.
- Perform aging studies to confirm shelf life and material integrity after sterilization.
- Use environmental conditioning to spot potential issues before releasing products.
- Maintain cleanroom discipline to prevent contamination during handling.
- Ensure graphics and labels withstand sterilization without fading or damage.
- Standardize work instructions for consistent loading and sterilization.
- Document material qualifications and compatibility with e-beam methods.
- Validate sealing processes and monitor them regularly.
These practices support the safety of medical devices with embedded electronics. They also help ensure that devices for wearable and diagnostic applications meet strict quality standards.
Regulatory Standards
Regulatory standards guide the safe and effective use of e-beam sterilization for medical devices with embedded electronics. International and national agencies set requirements for process validation, risk management, and quality control. The following table summarizes key standards in the United States and European Union:
| Standard | Description |
|---|---|
| ANSI/AAMI/ISO 11137 | Sets international rules for product, process, and installation qualification for electron-beam systems. |
| EN 552 | Offers additional guidelines for e-beam sterilization in the EU. |
| FDA’s Quality System Regulation (21 CFR Part 820) | Requires design controls, risk management, and post-market surveillance in the US. |
| EU Medical Device Regulation (EU MDR/IVDR) | Focuses on risk-based classifications and conformity assessments in the EU. |
| ISO 13485 | Provides a blueprint for quality management systems worldwide. |
| ISO 14971 | Addresses risk management for medical devices. |
Facilities must also obtain site licenses for e-beam systems, similar to other radiation equipment. State agencies issue these licenses, often completing the process quickly without public notice or special permits.
ISO 11137 outlines procedures for designing and validating radiation sterilization processes, including e-beam. This standard is essential for establishing a specific Sterility Assurance Level (SAL) after validation. Leading service providers follow these requirements to ensure that medical devices with embedded electronics meet global safety expectations. These standards support a wide range of applications, from implantable sensors to wearable electronics, by confirming that sterilization processes protect both device function and patient safety.
Conclusion
E-beam sterilization supports safe and effective processing of complex medical devices with embedded electronics. Process optimization and validation remain essential for wearable and electronic skin technologies. The method offers rapid, low-temperature sterilization, but some limitations exist:
| Limitation | Description |
|---|---|
| Penetration capabilities | E-beam sterilization lacks the penetration capabilities of EtO sterilization, making it unsuitable for complex or densely packaged devices. |
| High initial cost | The high initial cost of e-beam sterilization equipment can be a barrier for smaller manufacturers. |
The medical device sector expects strong growth in e-beam adoption due to technological advancements and a shift toward sustainable practices.
- The e-beam sterilization market is projected to grow at a CAGR of 11.3% from 2025 to 2032.
- Advancements in e-beam technology are contributing to its growing adoption in the medical device sector.
- There is a shift towards sustainable practices in sterilization methods, further promoting the use of e-beam sterilization.
E-beam sterilization continues to offer significant benefits for advanced medical devices, making it a valuable choice for manufacturers.
FAQ
How Does E-Beam Sterilization Differ from Gamma or Ethylene Oxide Methods?
E-beam sterilization uses high-energy electrons for rapid, low-temperature processing. Gamma uses radioactive sources and takes longer. Ethylene oxide relies on gas and requires aeration. E-beam avoids chemicals and radioactive materials, making it safer for sensitive electronics.
Can E-Beam Sterilization Damage Embedded Electronics?
E-beam sterilization can affect sensitive electronics if not properly controlled. Manufacturers select suitable materials and optimize dose levels. Most modern devices withstand the process when designed for e-beam compatibility.
What Types of Medical Devices Benefit Most from E-Beam Sterilization?
Wearable sensors, implantable devices, and electronic skin technologies benefit most. These products often contain heat-sensitive components. E-beam’s rapid, low-temperature process protects device function and material integrity.
Is E-Beam Sterilization Safe for Packaging Materials?
Most medical packaging materials tolerate e-beam sterilization well. Manufacturers test and qualify materials to ensure seals remain strong and packaging stays intact after exposure.
How Do Manufacturers Ensure E-Beam Sterilization Is Effective?
Manufacturers use validation protocols, including dosimetry mapping and microbial testing. They confirm that every device receives the correct dose and meets sterility requirements before market release.
