
Dose setting methods help manufacturers determine the radiation dose needed for medical device sterilization. The vdmax approach offers a flexible and conservative path for dose validation, supporting safety and regulatory compliance. Accurate dose setting prevents failures that may lead to product recalls.
- 48% of recalls resulted from lack of assurance in sterility.
- 45% of recalls involved non-sterility.
The vdmax method helps reduce these risks by enabling effective dose confirmation with reliable results.
Key Takeaways
- Accurate dose setting is crucial for medical device sterilization. It prevents under-sterilization, which can lead to infections, and over-sterilization, which may damage devices.
- The VDmax approach offers flexibility in dose validation. It allows manufacturers to confirm sterilization doses with fewer product units, reducing costs and time.
- Bioburden testing is essential for determining the correct sterilization dose. Regular monitoring helps maintain product safety and compliance with standards.
- Implementing best practices in VDmax can enhance sterilization effectiveness. Manufacturers should focus on sample selection, environmental control, and quality assurance.
- Ongoing education and adherence to ISO standards support successful sterilization processes. This ensures both regulatory compliance and public health safety.
Dose Setting in Medical Device Sterilization
What Is Dose Setting?
Dose setting defines the amount of radiation required to achieve effective sterilization of medical devices. This process ensures that each product receives a dose high enough to eliminate harmful microorganisms but not so high that it damages the device. In medical device sterilization, dose-setting plays a crucial role in balancing safety and product integrity. International standards, such as ISO 11137-1:2015, guide manufacturers in developing, validating, and controlling radiation sterilization processes.
The primary objectives of dose setting include:
- Establishing a maximum sterilization dose for product safety and functionality.
- Testing and considering material compatibility.
- Documenting the maximum dose to validate the sterilization process.
Why Dose Setting Matters?
Accurate dose-setting protects both patients and healthcare workers. It prevents under-sterilization, which can lead to infections, and over-sterilization, which may compromise device performance. Manufacturers must consider several critical parameters when selecting a dose-setting method for medical device sterilization.
| Critical Parameter | Description |
|---|---|
| Product Compatibility | Ensures that the sterilization method does not adversely affect the device’s materials and functionality. |
| Safety of the Sterilization Process | Considers both occupational safety for personnel and patient safety regarding sterilant residuals. |
| Impact on Product Functionality | Evaluates how sterilization methods may alter the device’s intended use or introduce harmful substances. |
Common Methods
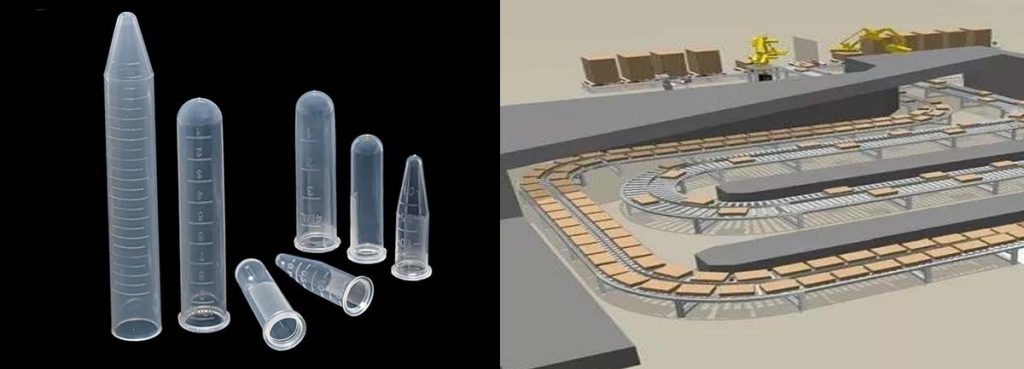
Manufacturers use several dose determination methods to set the correct sterilization dose. The most common approaches include the VDmax method, Method 1, and Method 2. The VDmax approach allows for flexible dose validation based on bioburden testing and supports different sterilization dose levels. Method 1 and Method 2 rely on statistical sampling and microbial inactivation data. Electron beam irradiation equipment often serves as a preferred technology for delivering precise doses during medical device sterilization. Each method aims to ensure that the sterilization process meets regulatory requirements and maintains product quality.
VDmax Approach Overview
Principles of VDmax
The vdmax approach builds on bioburden testing and the principles found in Method 1. Both methods aim to determine the correct sterilization dose for medical devices, but they differ in their requirements and efficiency. The vdmax method uses a streamlined process that requires fewer product units and focuses on practical sterility confirmation. Manufacturers select at least 40 systems for testing. They perform bioburden testing on 30 units, taking 10 from each of three different lots. After exposing 10 additional units to a low verification dose, they confirm sterility. This process helps ensure that the selected dose achieves the desired sterility assurance level.
| Aspect | Method 1 | VDmax Approach |
|---|---|---|
| Number of Units Required | Over 100 or 200 units | At least 40 systems |
| Bioburden Testing Units | Multiple dose analyses | 30 units (10 from each of three lots) |
| Sterility Confirmation | Not specified | 10 units after low dose exposure |
| Established Dosage Level | Not specified | 25 kGy or 15 kGy for plastic devices |
The vdmax approach efficiently addresses variability in product bioburden. It focuses on product characteristics and adapts to different levels of microbial contamination. This makes the method vdmax suitable for a wide range of medical devices.
| Method | Handling Variability in Bioburden | Focus on Product Characteristics |
|---|---|---|
| VDmax | Efficient | Yes |
| Method 1 | Less efficient | No |
| SIP | Justifiable under specific cases | No |
Flexibility in Dose Selection
The vdmax approach offers flexibility in selecting sterilization doses for different product types. Manufacturers can validate a standardized minimum sterilization dose of 25 kGy, which works well for many product lines. This flexibility benefits high-cost products and markets where 25 kGy is the accepted standard. The method vdmax also allows for the determination of a maximum dose based on material compatibility and product function. This flexibility supports product-specific vdmax applications, making it easier to adjust processing schedules and meet unique product needs.
Note: The vdmax approach supports both 25 kGy and 15 kGy doses, especially for plastic devices. This adaptability helps manufacturers maintain product quality while ensuring effective sterilization.
Product-specific vdmax validation ensures that each device receives the most appropriate dose. This approach reduces the risk of overexposure and helps maintain device performance. Manufacturers can confidently apply the method vdmax to a variety of products, knowing that the process supports both safety and efficiency.
Conservativeness and Safety
The vdmax method stands out for its conservative and safe approach to sterilization. It relies on the Standard Distribution of Resistances (SDR), which provides a strong safety margin. The method vdmax consistently delivers reliable results, even when microbial resistance varies. Over 500 verification dose experiments have shown no failures, highlighting the high level of safety associated with this approach.
| Evidence Type | Description |
|---|---|
| Conservative Basis | The vdmax method relies on the conservative Standard Distribution of Resistances (SDR). |
| Evaluation Outcomes | Consistent reliable results were observed across various microbial resistance distributions, particularly with resistances equal to or less than the SDR. |
| Safety Record | Around 500 verification dose experiments were conducted with no failures reported, indicating a high level of safety. |
The vdmax approach substantiates sterilization doses effectively, especially the minimum dose of 25 kGy. It provides high levels of sterility assurance, with no failures in verification dose experiments. International standards such as ISO 11137-2:2006 and AAMI TIR33:2005 recognize the method vdmax, linking sterilization doses to a sterility assurance level (SAL) of 10⁻³.
- The vdmax approach substantiates sterilization doses effectively, particularly a minimum dose of 25 kGy.
- High levels of sterility assurance are indicated, with no failures in verification dose experiments.
- The approach is included in ISO 11137-2:2006 and AAMI TIR33:2005, linking sterilization doses to a sterility assurance level (SAL) of 10⁻³.
Product-specific vdmax validation further enhances safety by tailoring the process to each device’s needs. This ensures that every product meets strict sterility requirements without unnecessary exposure to radiation.
Sterilization Process Steps with VDmax
The sterilization process using the vdmax approach follows a structured path. Each step ensures that medical devices meet strict sterility standards while maintaining product quality. Manufacturers and quality teams must pay close attention to every phase, from sample selection to final verification. This section outlines the essential steps and highlights practical considerations for successful implementation.
Sample Selection
Sample selection forms the foundation of the vdmax sterilization process. Manufacturers must choose representative samples from different production lots. This practice helps capture the natural variability in bioburden levels. ISO 11137 guidelines recommend specific sample sizes for dose validation. The table below summarizes the requirements for common dose establishment methods:
| Method | Sample Size (Total) | Conditions |
|---|---|---|
| VDmax15-35 | ≈ 46 samples | Bioburden of 1.5 CFU or higher, 15-35 kGy |
| Method 1 | ≈ 120 samples | Low sterilization dose (≤15 kGy) |
Manufacturers typically select at least 40 to 46 samples for vdmax validation. These samples should come from at least three different lots to ensure a robust assessment. Quality teams must document the lot numbers and maintain traceability throughout the sterilization process. Proper sample selection supports accurate dosimetry and reliable process validation.
Tip: Consistent sampling from multiple lots improves the reliability of the sterilization process and helps identify potential issues early.
Bioburden Testing

Bioburden testing measures the number of viable microorganisms present on each device before radiation sterilization. This step is critical for establishing the correct sterilization dose. The most common bioburden testing techniques and their detection limits appear in the table below:
| Testing Technique | Detection Limit |
|---|---|
| VDmax25 | 1,000 cfu/unit |
| VDmax15 | 1.5 cfu/product |
| Method 1 | Based on SDR |
| Method 2 | Based on resistance |
| ISO/TS 13004 | 17.5 to 35 kGy |
Manufacturers must validate the bioburden test method for each medical device. Validation ensures that the method recovers microorganisms effectively and does not inhibit their growth. Recovery data from validation testing may indicate the need for a recovery factor. Bioburden enumeration provides essential data for setting sterilization parameters and maintaining safety. Consistency in bioburden levels across lots is vital for achieving the desired sterility assurance level.
- The bioburden test method must be validated for each product.
- Validation ensures effective recovery of microorganisms.
- Recovery data may require a recovery factor.
Quality teams should monitor bioburden trends over time. Sudden changes in bioburden may signal issues in manufacturing or handling. Early detection allows for corrective action before the sterilization process begins.
Dose Validation
Dose validation confirms that the selected sterilization dose achieves the required sterility assurance level. The vdmax approach uses statistical analysis and microbial population assessments to validate the dose. The process involves counting the bioburden on the product and testing a sample at a low verification dose. The sample size for this step is typically 10 units, which provides a 1 in 10 probability of detecting a non-sterile unit. This contrasts with Method 1, which uses 100 units and a 1 in 100 probability.
- The vdmax 25 method, as described in ISO 11137, targets a 25 kGy dose.
- Statistical analysis ensures the sterilization dose is adequate.
- The goal is to achieve a Sterility Assurance Level (SAL) of 10⁻⁶.
Manufacturers must use accurate dosimetry to measure the radiation dose delivered to each sample. Dosimetry systems must be calibrated and traceable to national or international standards. Quality teams should review all dosimetry data before proceeding to the next step.
Note: A periodic dose audit can be completed within three to four weeks. The process includes irradiating samples and testing for sterility. Bioburden testing can occur during the two-week incubation period.
Verification
Verification serves as the final checkpoint in the vdmax sterilization process. This step confirms that the sterilization dose provides the intended level of sterility. The process includes three main actions:
- Bioburden test: Determines the quantity of viable microorganisms on or in the product before sterilization.
- Application of verification dose: Uses bioburden results to determine and apply the verification dose to products.
- Sterility test: Irradiated products undergo a sterility test, with acceptance criteria defined in ANSI/AAMI/ISO 11137-2.
Acceptance criteria are clear and straightforward:
- If one or no positive sterility samples are found, the sterilization dose is acceptable.
- If two or more positive sterility tests occur, the sterilization dose is not acceptable. Further action is required.
Quality teams must document all results and review any deviations from the expected outcome. Consistent verification ensures that the sterilization process remains effective and compliant with regulatory standards.
Manufacturers often face challenges such as resistance to change, lack of leadership support, and inconsistent processes. Addressing these issues requires strong leadership, comprehensive training, and standardized procedures.
The vdmax approach, when implemented correctly, provides a reliable and efficient path for radiation sterilization. Each step, from sample selection to verification, plays a vital role in ensuring product safety and regulatory compliance.
VDmax Pros and Cons
Benefits
The VDmax approach offers several advantages for medical device manufacturers.
- It has demonstrated safety and robustness for over a decade in substantiating radiation sterilization doses.
- Manufacturers can apply it across a wide range of bioburden levels and sterilization doses, which provides flexibility.
- The method uses only 10 product items in verification dose experiments, which helps reduce costs for high-value medical products.
- VDmax supports both higher and lower sterilization doses, making it suitable for many product types.
- Field evaluations at multiple facilities have confirmed the method’s versatility and reliability.
- Nearly 500 verification dose experiments have shown no failures, which highlights its high reliability.
- Smaller sample sizes mean less destructive testing and faster implementation, which benefits both cost and time.
Tip: Using VDmax can help maintain product quality by minimizing unnecessary exposure during sterilization.
Limitations
Despite its strengths, the VDmax approach has some limitations.
- Sometimes, it may require a higher sterilization dose compared to other methods, which could affect sensitive products.
- The method may not suit products with very high or highly variable bioburden.
- Some regulatory bodies may prefer alternative dose setting methods for specific device categories.
- Manufacturers must ensure strict adherence to sample selection and bioburden testing protocols to maintain quality.
| Method | Cost Implications |
|---|---|
| VDmax SD-S | Lower product consumption and cost savings |
| Method 1 | Higher validation costs due to larger sample sizes |
| Method 2 | Increased product use for validation |
Best Use Cases
The VDmax approach works best in certain scenarios:
- Substantiating sterilization doses for medical devices with consistent bioburden
- Healthcare products that have low bioburden
- Establishing minimum sterilization doses for products that require careful dose management
Manufacturers often choose VDmax when they need to balance product performance, cost, and quality. This method supports efficient sterilization validation and helps maintain high standards in device safety.
Practical Tips for VDmax Implementation
Best Practices
Manufacturers achieve the best results with the VDmax approach by following a systematic process. They start by assessing bioburden on sample items and prepare at least 40 samples from three different production lots. This ensures comprehensive testing and validation. In environments where bioburden control is critical, such as those producing healthcare products, these steps align with industry best practices.
- Select the sterilization method based on product material and bioburden levels.
- Implement an environmental monitoring program to control bioburden.
- Clean and store raw materials properly to prevent contamination.
- Establish clear procedures for personnel hygiene and gowning.
- Maintain strict housekeeping protocols and document all cleaning activities.
Tip: Manufacturers should determine the bioburden on the sample item proportion and submit samples for bioburden determination and validation testing. If bioburden falls below 30–50 CFUs per sample, alternative validation approaches may be more suitable.
Common Pitfalls
Some common pitfalls can hinder successful VDmax implementation. The table below outlines these challenges and strategies to avoid them:
| Pitfall | Avoidance Strategy |
|---|---|
| Treating security as an afterthought | Integrate security from the start of the development process. |
| Failing to foster a collaborative culture | Promote teamwork and open communication among all teams. |
| Relying solely on tools without skilled personnel | Ensure skilled personnel use tools and address complex threats. |
| Neglecting continuous monitoring and feedback | Maintain ongoing monitoring and feedback loops for real-time detection. |
| Ignoring compliance and regulatory requirements | Follow compliance standards to avoid breaches and financial losses. |
Manufacturers who address these pitfalls early can maintain process control and ensure microbicidal effectiveness.
Quality Assurance
Quality assurance plays a key role in ongoing compliance with VDmax dose setting requirements. Manufacturers should conduct quarterly dose audits to confirm the 25 kGy sterilization dose. If two positives occur during an audit, they must test 10 more samples. If no positives appear, the dose is confirmed. If three to six positives are found, the sterilization dose should be increased until an alternative method is chosen. If seven or more positives occur, manufacturers must select a different dose setting method.
| Activity | Description | Frequency |
|---|---|---|
| Bioburden Monitoring | Measure cleanliness to ensure no spikes in bioburden affect sterility. | Quarterly or more frequently |
| Sterility Testing | Test samples for sterility using the verification dose. | Based on initial validation |
| Dose Audits | Substantiate sterility claims post-validation. | Quarterly |
Manufacturers in healthcare must monitor bioburden and perform regular audits to maintain compliance and product safety.
Conclusion

Dose setting plays a vital role in medical device sterilization. The VDmax approach offers a proven method for achieving reliable and safe sterilization. Manufacturers who use VDmax can protect product quality and patient safety.
Ongoing education and strict adherence to best practices help ensure compliance and effectiveness.
By choosing the right dose setting method, manufacturers support both regulatory standards and public health.
FAQ
What Is the Purpose of Iso 11137 in Medical Device Sterilization?
Iso 11137 sets standards for radiation sterilization of medical devices. It guides manufacturers in dose setting, validation, and process control. The standard helps ensure devices meet safety and sterility requirements.
How Does Iso 11137 Support the VDmax Approach?
Iso 11137 provides detailed procedures for implementing the VDmax approach. It outlines sample selection, bioburden testing, and dose verification. Manufacturers rely on iso 11137 to validate sterilization doses and maintain compliance.
Why Is Bioburden Testing Important Under ISO 11137?
Bioburden testing measures microorganisms on devices before sterilization. ISO 11137 requires this step to determine the correct dose. Accurate bioburden data helps manufacturers achieve effective sterilization and meet regulatory standards.
Tip: Regular bioburden testing under ISO 11137 improves process reliability.
Can ISO 11137 Be Used for Different Sterilization Methods?
ISO 11137 applies to radiation sterilization, including gamma and electron beam methods. The standard covers dose setting, validation, and monitoring. Manufacturers use ISO 11137 to ensure consistent sterilization across various technologies.
What Are the Key Steps in ISO 11137 Dose Validation?
Manufacturers follow ISO 11137 for dose validation. Key steps include sample selection, bioburden testing, dose calculation, and verification. ISO 11137 ensures each step meets strict safety and quality requirements.
| Step | Description |
|---|---|
| Sample Selection | Choose representative samples |
| Bioburden Testing | Measure microorganisms |
| Dose Calculation | Determine sterilization dose |
| Verification | Confirm sterility |
