

Medical supply sterilization forms the backbone of modern infection control. Without proper sterilization, patients risk exposure to dangerous microorganisms during every procedure. In recent years, hospitals have adopted advanced technologies like UV-C light and antimicrobial coatings, which help reduce infection rates. The table below highlights global trends in medical sterilization and infection control:
| Aspect | Evidence Summary |
|---|---|
| Trends | Automation, AI, and advanced low-temperature sterilization improve quality and safety for patient care. |
| Impact on Infection Rates | Better sterilization practices lower infection rates worldwide, but gaps remain in some regions. |
Thorough cleaning before sterilization ensures that patients receive safe, sterile supplies, reducing the risk of infection in every healthcare setting.
Key Takeaways
- Sterilizing medical supplies kills all harmful germs, protecting patients and healthcare workers from infections during procedures.
- Proper cleaning before sterilization is crucial to remove dirt and biofilm that can block sterilization and cause infections.
- Different sterilization methods suit different supplies; choosing the right one keeps supplies safe without damage.
- Following strict cleaning and sterilization rules helps hospitals reduce infection rates and improve patient safety.
- Poor sterilization can cause serious infections, legal problems, and higher costs, so hospitals must maintain high standards.
Role of Sterilization
Foundation of Infection Control
The role of sterilization stands as the cornerstone of infection control in healthcare. Hospitals and clinics rely on sterile medical supplies to prevent the spread of infection among patients and staff. Medical supply sterilization eliminates all forms of microbial life, including bacteria, viruses, and fungi, from instruments and devices. This process ensures that supplies do not act as vectors for infectious agents, which is critical for patient safety.
The importance of sterilization becomes clear when considering the classification of medical instruments:
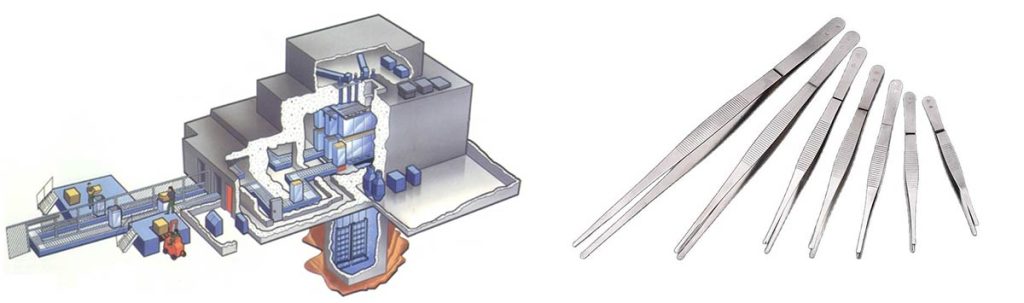
- Critical items, such as scalpels and forceps, penetrate skin or mucous membranes. These supplies require heat sterilization or chemical sterilants after thorough cleaning.
- Semicritical items, like dental handpieces, contact mucous membranes and must undergo heat sterilization or high-level disinfection between patients.
- Noncritical items pose the lowest risk and need only low-level disinfection.
The CDC emphasizes cleaning before sterilization and strict adherence to manufacturer instructions. This protocol underpins infection control in healthcare by eliminating microbial contamination on reusable supplies.
Scientific research confirms the effectiveness of sterilization in removing bacteria, viruses, and fungi from medical instruments. The following table compares common sterilization methods used for different types of supplies:
| Sterilization Method | Advantages | Disadvantages |
|---|---|---|
| Steam | Rapidly microbicidal; penetrates packaging and lumens; easy to monitor; nontoxic | Damages heat-sensitive instruments; potential rusting; risk of burns |
| Hydrogen Peroxide Gas Plasma | Safe for environment and personnel; no toxic residues; suitable for heat/moisture-sensitive items; simple operation | Cannot process cellulose or liquids; requires special packaging; potential toxicity at high levels |
| Ethylene Oxide (ETO) Gas | Penetrates packaging and lumens; compatible with most materials; simple to operate | Requires aeration to remove toxic residues; carcinogenic and flammable; lengthy cycle time |
| Vaporized Hydrogen Peroxide | Safe; no toxic residue; suitable for heat/moisture-sensitive items | Limited material compatibility data; not for liquids or cellulose; requires synthetic packaging |
Sterilization achieves a reduction of at least 10^6 colony forming units of the most resistant spores during a standard cycle. This level of sterility is necessary to prevent the transmission of pathogens such as hepatitis B virus and multidrug-resistant organisms. Each sterilization method is tailored to the type of supplies and their material compatibility, ensuring that all supplies used in patient care meet the highest standards of sterility.
Proper cleaning before sterilization is vital for the effectiveness of the process. Immediate cleaning after use prevents biofilm formation, which can shield pathogens from sterilization. Disassembling instruments exposes all surfaces to cleaning agents, removing residual debris. Using the correct cleaning solutions and following manufacturer instructions ensures that supplies are free from organic material that could compromise sterilization. Overloading cleaning or sterilization equipment can obstruct exposure to cleaning agents, reducing the effectiveness of sterilization and increasing the risk of infection.
A study found that vaporized hydrogen peroxide sterilization failed 76% of the time when instruments were not properly cleaned and remained soiled with blood or salts. This highlights the importance of cleaning in achieving true sterility. Quantitative studies show that cleaning methods can reduce residual protein contamination by over 99%, which is crucial for the importance of sterile medical supplies.
Protecting Patients and Staff
Sterile medical supplies protect both patients and healthcare staff from infectious diseases. The importance of sterilization extends beyond patient safety to include the well-being of everyone in the healthcare environment. Sterilization and disinfection of medical instruments eliminate or reduce microbial contamination, preventing surgical site and device-related infections. EO gas sterilization is effective against a broad range of pathogens and is suitable for heat- and moisture-sensitive devices, ensuring safety and compliance with infection control standards.
Maintaining a sterile healthcare environment through sterilization reduces the risk of healthcare-associated infections (HAIs). Sterile medical supplies complement other infection prevention measures, such as hand hygiene, personal protective equipment, vaccination, and infection control policies. Infection preventionists play a key role in implementing sterilization protocols and monitoring infection rates to improve patient and staff safety.
The impact of sterile medical device on infection control in healthcare is significant. By ensuring that all supplies are sterile before use, hospitals and clinics protect patients from exposure to harmful microorganisms. The importance of sterile medical supplies cannot be overstated, as even a single lapse in sterility can lead to infection outbreaks, increased healthcare costs, and patient harm.
The importance of sterility in healthcare settings lies in its ability to break the chain of infection transmission. Sterile supplies ensure that every patient receives care with the lowest possible risk of infection. The impact of medical sterilization on patient outcomes is profound, reducing the incidence of HAIs and improving overall healthcare quality.
Tip: Always follow manufacturer instructions for cleaning and sterilizing supplies. Proper technique ensures the highest level of sterility and protects both patients and staff from infection.
The role of sterilization in infection control in healthcare cannot be underestimated. The importance of sterile medical device, combined with rigorous cleaning and sterilization protocols, forms the foundation of safe patient care. The impact of these practices reaches every patient, every procedure, and every member of the healthcare team.
Infection Prevention
Breaking the Chain of Transmission
Infection prevention stands at the core of every healthcare facility’s mission to protect patients. Sterile medical supplies play a crucial role in breaking the chain of infection transmission. Every patient faces risks from pathogens present in the environment, on equipment, and on the hands of healthcare workers. Medical sterilization interrupts the steps that allow infections to spread.
The chain of infection consists of several key steps:
- Infectious agent: The pathogen that causes disease.
- Reservoir: Locations where pathogens live and multiply, such as people, animals, medical equipment, soil, or water.
- Portal of exit: How pathogens leave the reservoir, including open wounds, aerosols, coughing, or sneezing.
- Mode of transmission: The way pathogens spread, such as direct or indirect contact, ingestion, or inhalation.
- Portal of entry: How pathogens enter a new host, including broken skin, respiratory tract, mucous membranes, catheters, or tubes.
- Susceptible host: Individuals at risk, especially those with weakened immune systems or invasive devices.
Sterilization and disinfection of supplies target these steps by eliminating pathogens from surfaces and equipment. Hospitals use routine cleaning and disinfection protocols to remove organic matter and debris from supplies. This process prevents microorganisms from being shielded during sterilization. Mechanical and manual cleaning methods ensure thorough removal of contaminants from surgical instruments and other supplies.
Note: Proper handling, packaging, and transport of sterile medical supplies prevent recontamination before use. This step is essential for maintaining the importance of sterility throughout the supply chain.
Environmental cleaning and maintenance of operating rooms, including ventilation and regular equipment checks, further reduce microbial contamination. These combined protocols break the chain of infection, protecting every patient who enters a healthcare facility.
Sterile Medical Supplies in Procedures
Sterile medical supplies are essential for every procedure, from minor wound care to complex surgeries. The use of sterile medical equipment and supplies prevents cross-contamination and reduces the risk of healthcare-associated infections. Hospitals rely on strict sterilization protocols to ensure that every supply used in patient care meets the highest standards of sterility.
A meta-analysis pooling data from multiple studies found that implementing sterile supply center management protocols reduced the odds of healthcare-associated infections by 70%. Another analysis showed an 85% decrease in adverse events related to sterilization and supply management. Individual studies reported dramatic drops in infection rates, such as a reduction from 4.44% to 0.64% after introducing quality improvement cycles for sterilization.
The impact of sterile medical supplies on patient safety is clear. Lower surgical site infection rates and reduced detection of pathogenic bacteria have been documented in groups using improved sterilization and supply management. Improvements in disinfection quality, hand hygiene, and staff knowledge consistently lead to lower infection rates and higher satisfaction among healthcare workers.
Hospitals use the Spaulding Classification to determine the required level of sterilization or disinfection for each type of supply:
| Classification | Example Supplies | Required Process |
|---|---|---|
| Critical | Surgical instruments | Sterilization |
| Semicritical | Endoscopes, respiratory equipment | High-level disinfection or sterilization |
| Noncritical | Blood pressure cuffs, stethoscopes | Low-level disinfection |
Sterile medical supplies protect patients from hospital-acquired infections during every procedure. The importance of sterile medical supplies extends to all areas of patient care, including surgery, wound care, and invasive device management. Hospitals that prioritize the role of sterile medical supplies see significant reductions in healthcare-associated infections and HAIs.
Tip: Staff should always follow manufacturer instructions for cleaning and sterilizing supplies. This practice ensures the highest level of sterility and supports infection prevention efforts.
The impact of medical sterilization on reducing healthcare-associated infections cannot be overstated. Hospitals that invest in advanced sterilization methods, such as electron beam sterilization, further enhance the safety of their supplies. The importance of sterile medical supplies lies in their ability to prevent cross-contamination, protect patients, and support the overall goal of infection prevention.
Sterile medical equipment and supplies form the foundation of patient safety. Every patient deserves care with sterile supplies, free from the risk of infection. The importance of sterility in healthcare settings ensures that hospitals can continue preventing hospital-acquired infections and improving outcomes for every patient.
Risks of Poor Sterilization
Outbreaks and HAIs
Poor sterilization of medical supplies creates serious risks for every patient in healthcare settings. When supplies do not meet strict sterilization standards, infection can spread quickly. Healthcare-associated infections often result from contaminated supplies, especially when invasive procedures use central lines, catheters, or ventilators. The most common healthcare-associated infections linked to poor sterilization include central line-associated bloodstream infections, catheter-associated urinary tract infections, surgical site infections, and ventilator-associated pneumonia. These infections increase patient morbidity and mortality, raising healthcare costs and reducing the quality of care.
Outbreaks in hospitals frequently involve pathogens such as Staphylococcus aureus, Pseudomonas species, and Klebsiella species. These organisms thrive on improperly sterilized supplies and can infect vulnerable patients. Medical sterilization failures allow pathogens to persist on supplies, leading to hospital-acquired infections and healthcare-associated infections. The complexity of healthcare environments and the high number of supplies used for each patient make infection control challenging. When supplies remain contaminated, the impact on patient safety is immediate and severe.
Common errors in sterilization processes, such as dirty or missing supplies, often occur due to inexperienced or non-certified sterile processing technicians. These errors cause surgical delays, increase anesthesia time, and raise the risk of surgical site infections for every patient. Visualization failures during inspection and assembly of supplies account for most errors, leading to operational inefficiencies and increased infection risk. The impact of these mistakes extends to patient anxiety, surgeon dissatisfaction, and regulatory scrutiny.
Legal and Financial Consequences
The consequences of inadequate sterilization reach far beyond patient health. Healthcare facilities have legal and ethical duties to ensure all supplies undergo proper sterilization. Failure to comply exposes hospitals to malpractice lawsuits when patients develop infections from unsterilized supplies. Regulatory bodies can impose fines, sanctions, and penalties for violations of sterilization standards. Hospitals may lose accreditation, suffer reputational damage, and face significant financial settlements.
Improper sterilization also leads to indirect financial burdens. Canceled surgeries, increased infection control costs, and longer hospital stays for affected patients drive up expenses. Use of expired or improperly sterilized supplies can trigger legal actions, including fines and lawsuits. Regulatory agencies like the FDA enforce strict guidelines, and non-compliance results in severe penalties. The impact on hospital finances includes the cost of replacing supplies, addressing adverse outcomes, and managing reputational harm. Poor supply management reduces patient trust and referrals, further affecting the institution’s bottom line.
The consequences of inadequate sterilization highlight the critical role of medical sterilization in protecting every patient. Hospitals must prioritize the proper cleaning, inspection, and sterilization of all supplies to prevent infection, avoid legal action, and maintain high standards of patient care. The impact of poor sterilization practices can devastate both patient outcomes and healthcare facility operations.
Medical Supply Sterilization Methods
Steam and Heat-Based Techniques
Steam sterilization remains a cornerstone in medical supply sterilization. Hospitals use autoclaves to expose surgical instruments and other supplies to high-pressure steam at 121–134°C. This process quickly kills microbes by hydrolyzing and coagulating proteins. Steam cycles last between 3 and 15 minutes, making them efficient for large volumes of sterile medical equipment. Steam works best for heat-resistant supplies, such as metals, durable plastics, and rubber. However, it cannot process electronics or heat-sensitive materials. Dry heat sterilization offers an alternative for supplies like powders, oils, and some polymers. This method penetrates deeply and avoids corrosion, but it requires higher temperatures and longer cycles. Dry heat does not leave toxic residues and is cost-effective for certain sterile medical supplies.
| Technique | Advantages | Limitations |
|---|---|---|
| Steam | Fast, effective, low cost, eco-friendly | Damages heat-sensitive supplies, electronics |
| Dry Heat | No toxic residue, deep penetration, no corrosion | Slow, high energy, not for all supplies |
Note: Steam and dry heat sterilization both ensure the safety of sterile medical equipment, but each method fits specific types of supplies.
Electron Beam Sterilization
Electron beam sterilization uses high-energy electron beams to irradiate supplies. This method sterilizes surgical instruments and sterile medical equipment within seconds. It is especially effective for thermo-labile and highly functionalized supplies, such as those containing polymers or electronics. Hospitals can use electron beam sterilization for just-in-time processing, reducing storage needs for sterile medical supplies. The process inactivates even radiation-resistant pathogens, including Bacillus pumilus and Pseudomonas aeruginosa. Supplies retain their biocompatibility and electronic function after repeated cycles. Miniaturized electron-beam sources allow on-site sterilization of complex supplies, making this method suitable for hospitals and clinics.
Choosing the Right Method
Selecting the best sterilization method depends on the type of supplies, their material, and intended use. Critical supplies, such as surgical instruments, require the highest level of sterility. Steam sterilization offers a cost-effective solution for most metals and heat-resistant supplies. For supplies with embedded electronics or sensitive polymers, electron beam sterilization or chlorine dioxide sterilization provide effective alternatives. Ethylene oxide sterilization suits heat- and moisture-sensitive supplies but involves higher costs and environmental risks. Regulatory standards from agencies like the FDA and WHO guide medical equipment sterilization choices. Hospitals must also consider environmental impact, cost, and supply compatibility. Proper cleaning before sterilization remains essential for all supplies to ensure true sterility.
Tip: Always match the sterilization method to the supply’s material and function to maintain the integrity of sterile medical supplies and reduce infection risk.
Compliance and Best Practices
Regulatory Standards
Healthcare facilities must follow strict regulatory standards to ensure every patient receives sterile supplies. International organizations, such as the World Health Organization, provide guidance on infrastructure, procedures, and quality control for sterilization. In the United States and Europe, regulatory authorities enforce compliance with ISO standards and local regulations. The following table summarizes key standards and authorities:
| Region | Regulatory Authority / Standard | Description |
|---|---|---|
| United States | EPA, ISO 11135, ISO 11137 | Rules for ethylene oxide emissions, radiation sterilization, and validation of sterilization |
| Europe | EU MDR, ISO 17665, ISO 11607 | Harmonized standards for moist heat sterilization and sterile packaging |
| International | ISO 17664, ISO 11737-2 | Cleaning, disinfection, sterilization, and microbiological testing requirements |
| Certification | TÜV SÜD | Conformity assessments, audits, and validation for global compliance |
Manufacturers must validate sterilization processes and maintain documentation. Facilities must routinely monitor sterilization cycles and packaging integrity. These steps form the foundation of a comprehensive sterilization program and protect patient safety.
Role of Sterile Processing Technicians
Sterile processing technicians play a vital role in every comprehensive sterilization program. They clean, disinfect, and sterilize supplies, ensuring each item meets strict standards before reaching the patient. Their responsibilities include:
- Decontaminating and inspecting supplies for cleanliness and function.
- Assembling and packaging instrument trays tailored to surgical needs.
- Monitoring sterilization cycles with biological and chemical indicators.
- Maintaining detailed records for regulatory compliance.
- Delivering sterile supplies to healthcare teams, supporting surgical efficiency.
Technicians work in specialized departments that separate contaminated and clean areas, reducing infection risks for every patient. Their attention to detail and knowledge of medical sterilization directly impact patient safety and surgical outcomes.
Maintaining Sterile Environments

Hospitals and clinics must maintain sterile environments to protect every patient. Best practices include:
- Strict hand hygiene before and after handling supplies or patient contact.
- Regular disinfection of high-touch surfaces in operating rooms and patient care areas.
- Proper storage of sterile supplies in well-ventilated, dust-free areas.
- Labeling supplies with sterilization dates and monitoring packaging for damage.
- Comprehensive staff training and competency testing in sterilization protocols.
- Routine infection control rounds and quality control programs to monitor compliance.
A comprehensive sterilization program requires ongoing education, systematic checks, and accountability. Facilities that prioritize effective sterilization practices reduce infection risks and improve patient safety. Every step, from cleaning to storage, ensures that supplies remain sterile and ready for patient care.
Conclusion
Sterile supplies form the foundation of infection prevention and patient safety. Strict adherence to cleaning and sterilization protocols reduces infection rates, improves the impact on patient safety, and ensures every patient receives the highest standard of care. Ongoing education in sterilization best practices enhances staff expertise and supports consistent sterile supply management. Investment in advanced technologies, such as electron beam sterilization, delivers a positive impact by protecting patient health and optimizing resource use. Healthcare professionals should prioritize sterile supplies to maximize the impact on patient safety and improve outcomes for every patient.
